January 2021 Marks the 53rd Anniversary for the First Heart Transplant in the United States
January 6, 2021, marks the 53rd anniversary of the first adult heart transplant in the United States. It was performed at Stanford Hospital by Norman Shumway, MD, PhD, who is considered the father of heart transplantation and was one of the pre-eminent heart surgeons of his time. Shumway and his research team developed the standard surgical technique for heart transplantation that’s still in use today.
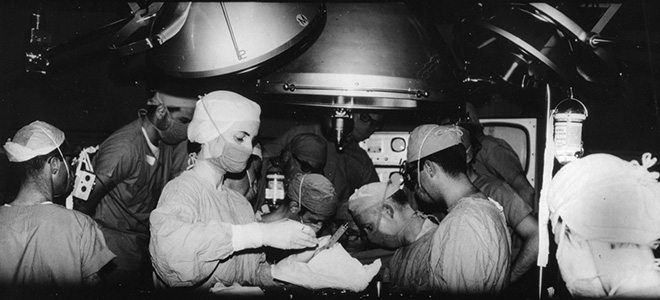
Norman Shumway (seated, right center) performed the first adult heart transplant in the United States on Jan. 6, 1968. Edward Stinson (seated, left center) assisted in the landmark surgery. Photo courtesy of Stanford Medical History Center.
Before Lucile Packard Children’s Hospital Stanford opened in 1991, Stanford pioneered the development of cardiac transplantation and therapies for children with end-stage heart failure. The first successful pediatric heart transplant at Stanford was done over 35 years ago, and we have been refining pediatric heart-transplant techniques ever since.
That historic pediatric heart transplant was performed on Elizabeth Craze, who was 2 years and 10 months old at the time. Craze, now 38, still has that same heart beating in her chest. Before the surgery at Stanford Hospital, Craze’s doctors faced a great deal of uncertainty. They didn’t even know if the donor heart, which came from a little girl in Utah who had died in a car crash, would grow with Craze or not.

Elizabeth Craze, was the first pediatric heart transplant recipient at Stanford. Photo courtesy of Craze family.
It did, and last time we connected with Craze she was doing well. She married in 2014 and a few years later she got a job at a Palo Alto startup, where she was a paralegal on the intellectual property team.
The success of her surgery paved the way for Packard Children’s to become a leader in the field, and on November 7, 2017, a team of pediatric specialists in the Betty Irene Moore Children’s Heart Center performed the 400th pediatric heart transplant at Stanford.
The recipient of the 400th transplant was 16-year-old Danny Yang of Marysville, California. Yang’s mother, Lisa Vue, expressed gratitude to the hospital’s doctors and nurses, who have cared for Danny since he and his family arrived at Packard Children’s in July because his heart was failing. Danny was born with a congenital heart condition called hypoplastic right heart syndrome, which left him without a right ventricle capable of pumping blood to his lungs. At the age of four, he received a corrective surgery known as a Fontan procedure. However, in his teenage years he developed chronic systolic and diastolic heart failure and required intravenous medications to maintain his circulation. As an associated consequence of his severe Fontan heart failure, he also developed liver disease, which doctors at Packard Children’s diagnosed in July 2017. His liver failure meant that he would need both a heart and liver transplant, which he received on November 7, 2017.
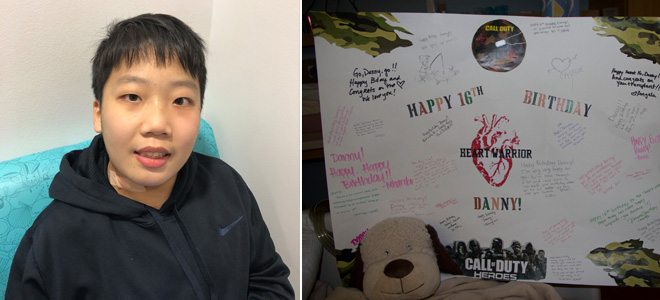
Danny Yang, 400th heart transplant recipient at Lucile Packard Children’s Hospital Stanford. Photo courtesy of family.
Multiple organ transplants require multidisciplinary collaboration across care teams specializing in each organ as well as pediatric anesthesiologists and pediatric intensivists. The complex care needs of patients like Danny are exactly what Packard Children’s Transplant Center is uniquely prepared to manage. Danny recovered well, and was discharged from the hospital in December 2017 to the Ronald McDonald House at Stanford where his mom and Danny’s two sisters resided before going home.
Advancing treatment and research for pediatric heart failure
Stanford has also been a pioneer in the field of heart pumps, also known as ventricular assist devices (VADs), which offer patients a “bridge” to heart transplantation. VADs help the heart move blood through the body and keep pediatric patients with severe heart failure stable so they can safely wait for a donor heart to become available. In addition to improving survival, a VAD alleviates many of the symptoms of heart failure, including trouble breathing, severe fatigue, nausea and vomiting, by ensuring enough blood can get to the body’s vital organs when the heart is weak.
In 2004, Packard Children’s was one of the very first U.S. hospitals to use the Berlin Heart, an external heart pump which until that time had been used primarily in Europe. Under the direction of David Rosenthal, MD, professor of pediatrics, Packard Children’s petitioned the U.S. Food and Drug Administration (FDA) to import the device from Germany for a 3-month-old patient, who was then one of the youngest children in the world to receive the pump. This little boy did well and received a heart transplant after 55 days of VAD support. The novel use of the Berlin Heart in this child ended up as a front page story in The New York Times and it served to catalyze interest in the device across the United States. Stanford faculty provided important leadership for a subsequent multisite clinical trial of the Berlin Heart, which led to its approval for use in children by the FDA in 2011.
Today, Stanford Medicine Children’s Health has one of the busiest pediatric VAD programs in the country and is pioneering use of smaller portable “durable VADs” that allow children to await transplant outside of the hospital and, in some cases, help them avoid transplant altogether. The result for many patients is a higher quality of life and better outcomes following transplantation. Having a heart pump can give transplant doctors more time to find a heart that is the best match for a patient. Also, since the pump allows a patient to breathe comfortably, engage in exercise and tolerate optimal nutrition, the patient becomes a better candidate for a heart transplant.

Ziyan Liu. Photo courtesy of family.
Eleven-year-old Ziyan Liu was born with single-ventricle congenital heart disease, and is one of only a small handful of patients with this type of heart defect to have been supported on a VAD. This device meant that she was able to wait for two years on the transplant list, and most of that time outside of the hospital. Ziyan received her heart transplant in July 2017 and she recovered well. Before her transplant, she was unable to participate fully in physical education in school due to her condition. Within five months of her transplant, she ran the mile at school, and she continued to run weekly afterwards.
The spirit of Stanford innovation continues
From the first transplant performed by Dr. Shumway in 1968 to one of the first pediatric heart transplants performed 35+ years ago and the thousands performed worldwide since, treatments for advanced heart failure will only continue to progress with innovations in technology and research. In 2017, Christopher Almond, MD, a pediatric cardiologist and associate professor of pediatrics at the Stanford University School of Medicine, began leading the first clinical trial in humans of the Jarvik 2015, an implantable device that is as long as a paperclip and is meant to replace the Berlin Heart. The longer-term goal for the Jarvik 2015 device is to allow smaller patients to go home with the device to wait for their heart transplant instead of the current practice of keeping them hospitalized on the Berlin Heart.

Photo courtesy of Jarvik Heart Inc.
“With tens of thousands of lives saved through heart transplantation, the work launched by Dr. Shumway has truly been transformative across the globe,” said Rosenthal. “Lucile Packard Children’s Hospital Stanford is proud to acknowledge the legacy of this remarkable surgeon and continues to advance the field that Dr. Shumway began 53 years ago.”
Connect with us:
Download our App: