Contact us
If you would like to learn more or if you are ready to make an appointment, please call or email our team.
Nicholas DeHart was 8 years old when he decided to join his school’s band. He chose the clarinet, a wind instrument. Normally, this wouldn’t be a big deal, but to his family and doctors, it marked a triumph. That’s because Nicholas was born without a pulmonary artery, the vessel that carries blood from the heart to the lungs for oxygenation.
Lifelong care from the Pulmonary Artery Reconstruction program at Lucile Packard Children’s Hospital Stanford has helped Nicholas achieve more than anyone might ever have imagined. Nicholas, now 13, recently ran the fastest mile in his class and was a first pick for the flag football team at his school in South Carolina, where he was born.
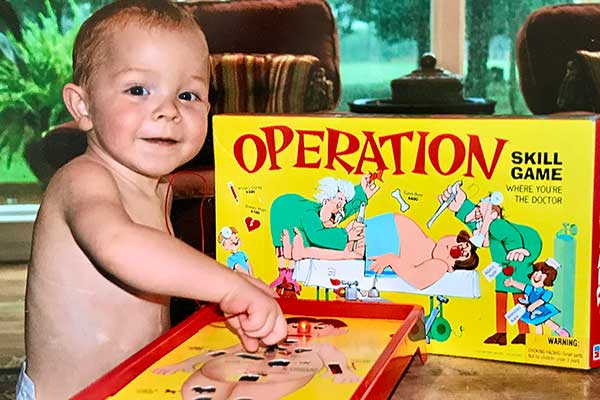
Nicholas looked healthy and robust as a newborn in May 2003. To compensate for his missing pulmonary artery, Nicholas, as a fetus, had developed several major aortopulmonary collateral arteries. These tiny, fragile blood vessels carried blood from his heart to his lungs, but they would not sustain him for long.
 Doctors soon diagnosed him with a complex congenital (meaning present at birth) heart condition called tetralogy of Fallot with pulmonary atresia. Tetralogy of Fallot, occurring in about 1 out of every 1,000 babies, involves four related defects of the heart. When the condition also includes pulmonary atresia, that means the patient has an added complication of a defective — or, as in Nicholas’s case, absent — pulmonary valve. Nicholas, who had the most complex type of tetralogy of Fallot, was missing not only a pulmonary valve but also the pulmonary arteries.
Doctors soon diagnosed him with a complex congenital (meaning present at birth) heart condition called tetralogy of Fallot with pulmonary atresia. Tetralogy of Fallot, occurring in about 1 out of every 1,000 babies, involves four related defects of the heart. When the condition also includes pulmonary atresia, that means the patient has an added complication of a defective — or, as in Nicholas’s case, absent — pulmonary valve. Nicholas, who had the most complex type of tetralogy of Fallot, was missing not only a pulmonary valve but also the pulmonary arteries.
Nicholas’s mother, Stephanie DeHart, a nurse anesthetist in South Carolina, got right to work investigating which medical teams across the country might be the most qualified to treat her baby. That’s when she found Frank Hanley, MD, director of the Betty Irene Moore Children’s Heart Center at Packard Children’s and chief of pediatric heart surgery at the hospital.
“Other doctors I spoke to had done one or two of these repairs,” said Stephanie. “Dr. Hanley was the only one who had done more than a hundred — more than anyone else in the field.”
Dr. Hanley, who is also a professor of cardiothoracic surgery at the Stanford University School of Medicine, developed a single-stage surgical repair for tetralogy of Fallot with pulmonary atresia. Before Hanley’s advance, surgeons would repair this complex condition in multiple surgeries over months or years. But Hanley’s approach of carefully opening each tiny collateral artery lengthwise and stitching them together to create a new pulmonary artery — a procedure called unifocalization — condensed the treatment into one revolutionary 12-hour surgery.
“In each patient, the defect has a unique presentation,” explains Hanley. The majority of patients — about 70 percent — qualify for the single-stage repair. “Nicholas was in the ten percent of patients whose condition is so complex that it requires three surgeries to get to the full cardiac repair.”
Dr. Hanley and his team did Nicholas’s first surgery, an 11-hour left-lung unifocalization, in November 2003. Nicholas’s right-lung unifocalization, which took 12 hours, happened six weeks later. Then, in April 2004, Nicholas underwent his third surgery in six months. In this final procedure, Dr. Hanley repaired the four related heart defects that make up tetralogy of Fallot and connected the heart to the reconstructed main pulmonary artery.
Hanley and his team have a 98 percent success rate with these surgical repairs — whether they are one stage or more — because they follow a strict protocol. “Even for patients like Nicholas, where it takes three operations to get there, we still use very strict criteria for doing the ultimate cardiac repair,” says Dr. Hanley. “We only do it when we’re pretty much guaranteed that the patient’s blood pressure is going to be adequate. In this way, we can expect Nicholas’s outcome to be similar to most of the other patients, even in his complex category.”
 “Surgery that is done early in life is unique here, and the outcomes are uniquely outstanding,” says Doff McElhinney, MD, medical director of the Pulmonary Reconstruction program at Packard Children’s and a professor of both cardiothoracic surgery and pediatrics at Stanford University’s School of Medicine.
“Surgery that is done early in life is unique here, and the outcomes are uniquely outstanding,” says Doff McElhinney, MD, medical director of the Pulmonary Reconstruction program at Packard Children’s and a professor of both cardiothoracic surgery and pediatrics at Stanford University’s School of Medicine.
“But it’s not a curative operation or series of operations. Patients continue to need ongoing evaluation and care. Some of that care will involve other procedures, such as replacement of the pulmonary valve conduits that are used during their repair early in life. Sometimes, those later procedures are performed surgically, and sometimes they’re performed with a transcatheter pulmonary valve, like the Melody valve, which was the most recent procedure Nicholas underwent here.”
Dr. McElhinney adds that even a successfully repaired heart with excellent function may still appear unusual, anatomically speaking. So, kids like Nicholas require a specially trained eye for follow-up care. “There’s a familiarity and an experience with the lesion overall that helps us to make judgments about what kind of abnormality matters and what doesn’t,” says McElhinney.
That unique knowledge kept the DeHart family returning to Packard Children’s for Nicholas’s major care needs over the years, including the replacement of his pulmonary artery in 2007 and several catheterizations. Most recently, in August 2016, Dr. McElhinney and his team used a catheter to implant Nicholas’s Melody valve — a valve that is placed without opening the heart and which allows the original surgically implanted valve to last longer, hopefully for many more years.
Over the last year, Packard Children’s has enhanced its Pulmonary Artery Reconstruction program, inspired by patients like Nicholas. Jennifer Shek, a dedicated nurse practitioner, serves as the program coordinator and helps to coordinate referrals and care for patients who come from all around the world to receive the unique care offered here.
“We’re working to understand and address the lifetime course of this disease more effectively and more comprehensively for these patients,” says Dr. McElhinney. “We now play a more active role with the family and their physician before they come here for their first surgery. And we’re establishing a more in-depth and extended relationship with each patient and family to help foster and bolster their experience before they arrive, when they’re here, and after they’ve gone home — which is often to another state or even country.”
Last year, Nicholas traded in his clarinet for a trumpet, and he also took up acting and voice lessons. “Nicholas is a delightful boy — funny, sweet, active and adventurous,” says Dr. McElhinney. “He’s a wonderful example of how kids living with heart disease can be everything. As a cardiologist or cardiac surgeon, that’s incredibly rewarding.”
Connect with us:
Download our App: