Childhood Brain Stem Glioma Treatment (PDQ®)
General Information About Childhood Brain Stem Glioma
Childhood brain stem glioma is a disease in which benign (noncancer) or malignant (cancer) cells form in the tissues of the brain stem.
The
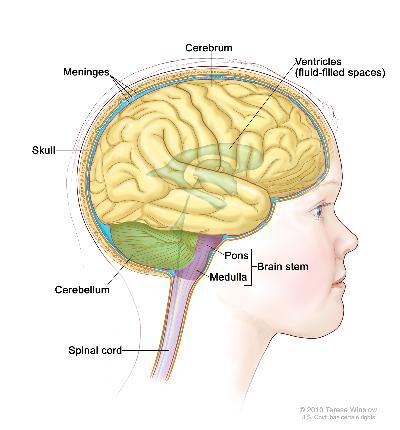
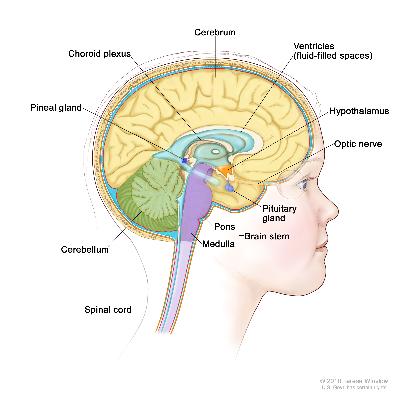
Anatomy of the brain, showing the cerebrum, cerebellum, brain stem, and other parts of the brain. | Anatomy of the inside of the brain, showing the pineal and pituitary glands, optic nerve, ventricles (with cerebrospinal fluid shown in blue), and other parts of the brain. |
The
This summary refers to the treatment of
Childhood Brain and Spinal Cord Tumors Treatment Overview
The cause of most childhood brain tumors is unknown.
The symptoms of childhood brain stem glioma vary and often depend on the child’s age and where the tumor is located.
The following symptoms and others may be caused by a brain stem glioma. Other conditions may cause the same symptoms. A doctor should be consulted if any of these problems occur:
Loss of balance and trouble walking.
Vision and hearing problems.
Morning headache or headache that goes away after
vomiting .Nausea and vomiting.Unusual sleepiness or change in energy level.
Tests that examine the brain are used to detect (find) childhood brain stem glioma.
The following
CT scan (CAT scan): A procedure that makes a series of detailed pictures of areas inside the body, taken from different angles. The pictures are made by a computer linked to anx-ray machine. Adye may beinjected into avein or swallowed to help theorgans or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography.MRI (magnetic resonance imaging) withgadolinium : A procedure that uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the brain andspinal cord . A substance called gadolinium is injected into a vein. The gadolinium collects around the cancer cells so they show up brighter in the picture. This procedure is also called nuclear magnetic resonance imaging (NMRI).
Some childhood brain stem gliomas are diagnosed and removed in surgery.
If the tumor has not spread widely within the brain stem or has not been
Certain factors affect prognosis (chance of recovery) and treatment options.
The
The type of brain stem glioma.
Where the tumor is found in the brain and if it has spread within the brain stem.
Whether or not the child has a condition called
neurofibromatosis type 1 .Whether the tumor has just been diagnosed or has
recurred (come back).
Stages of Childhood Brain Stem Glioma
The plan for cancer treatment depends on whether the tumor is in one area of the brain or has spread throughout the brain.
There is no standard staging system for childhood
Diffuse intrinsic
pontine glioma is a tumor that has spread widely throughout thebrain stem . Abiopsy is usually not done for this type of brain stem glioma and it is not removed bysurgery . A diffuse intrinsic pontine glioma is usuallydiagnosed usingimaging studies.Focal or
low-grade glioma is a tumor that is in one area of the brain stem. A biopsy may be done and the tumor removed during the same surgery.
There are three ways that cancer spreads in the body.
The three ways that cancer spreads in the body are:
Through
tissue . Cancerinvades the surrounding normal tissue.Through the
lymph system . Cancer invades the lymph system and travels through thelymph vessels to other places in the body.Through the
blood . Cancer invades theveins andcapillaries and travels through the blood to other places in the body.
When cancer
The information from tests and procedures done to detect (find) childhood brain stem glioma is used to plan cancer treatment.
Some of the tests used to detect childhood brain stem glioma are repeated if the tumor is removed by surgery. (See the General Information section.) This is to find out how much tumor remains after surgery and plan further treatment.
Recurrent Childhood Brain Stem Glioma
Treatment Option Overview
There are different types of treatment for children with brain stem glioma.
Different types of treatment are available for children with
Because cancer in children is rare, taking part in a clinical trial should be considered. Some clinical trials are open only to patients who have not started treatment.
Children with brain stem glioma should have their treatment planned by a team of health care providers who are experts in treating childhood brain tumors.
Treatment will be overseen by a
Neurosurgeon .Neuropathologist .Radiation oncologist .Neuro-oncologist .Neurologist .Rehabilitation specialist .Neuroradiologist .Endocrinologist .Psychologist .
Childhood brain and spinal cord tumors may cause symptoms that begin before diagnosis and continue for months or years.
Childhood brain and
Some cancer treatments cause side effects months or years after treatment has ended.
These are called
Physical problems.
Changes in mood, feelings, thinking, learning, or memory.
Second cancers (new types of cancer).
Some late effects may be treated or controlled. It is important to talk with your child's doctors about the effects cancer treatment can have on your child. (See the
Five types of standard treatment are used:
Surgery
Radiation therapy
Radiation therapy to the brain can affect growth and development in young children. Certain ways of giving radiation therapy can help keep radiation from damaging healthy
Conformal radiation therapy is a type of radiation therapy that uses a computer to make a 3-dimensional (3-D) picture of thetumor and shapes the radiation beams to fit the tumor. This allows a highdose of radiation to reach the tumor and causes less damage to normal tissue around the tumor.Hyperfractionated radiation therapy is radiation treatment in which the total dose of radiation is divided into small doses and the treatments are given more than once a day.
The way the radiation therapy is given depends on the type and
Several months after radiation therapy to the brain,
Chemotherapy
Chemotherapy is a cancer treatment that uses
Because radiation therapy to the brain can affect growth and brain development in young children, clinical trials are studying ways of using chemotherapy to delay or reduce the need for radiation therapy.
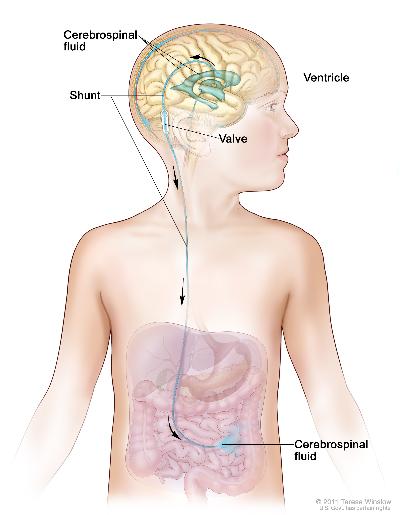
Cerebrospinal fluid diversion
Watchful waiting
New types of treatment are being tested in clinical trials.
This summary section describes treatments that are being studied in clinical trials. It may not mention every new treatment being studied. Information about clinical trials is available from the NCI Web site.
Radiation therapy with radiosensitizers
Patients may want to think about taking part in a clinical trial.
For some patients, taking part in a
Many of today's standard treatments for cancer are based on earlier clinical trials. Patients who take part in a clinical trial may receive the standard treatment or be among the first to receive a new treatment.
Patients who take part in clinical trials also help improve the way cancer will be treated in the future. Even when clinical trials do not lead to effective new treatments, they often answer important questions and help move research forward.
Patients can enter clinical trials before, during, or after starting their cancer treatment.
Some clinical trials only include patients who have not yet received treatment. Other trials test treatments for patients whose cancer has not gotten better. There are also clinical trials that test new ways to stop cancer from
Clinical trials are taking place in many parts of the country. See the Treatment Options section that follows for links to current treatment clinical trials. These have been retrieved from
Follow-up tests may be needed.
Some of the tests that were done to
Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your condition has changed or if the cancer has
Treatment Options for Childhood Brain Stem Glioma
A link to a list of current
Untreated Childhood Brain Stem Glioma
Untreated childhood
Some of the treatments being studied in
Radiation therapy with a
radiosensitizer .
Standard treatment of focal or
Surgery with or without radiation therapy, which may be followed byadjuvant chemotherapy .Cerebrospinal fluid diversion followed bywatchful waiting .
Treatment of brain stem glioma in children with
Check for U.S. clinical trials from NCI's list of cancer clinical trials that are now accepting patients with untreated childhood brain stem glioma. For more specific results, refine the search by using other search features, such as the location of the trial, the type of treatment, or the name of the drug. General information about clinical trials is available from the NCI Web site.
Recurrent Childhood Brain Stem Glioma
Treatment of
Treatment of recurrent focal or
Surgery .Radiation therapy .Chemotherapy .A clinical trial of a new treatment.
Check for U.S. clinical trials from NCI's list of cancer clinical trials that are now accepting patients with recurrent childhood brain stem glioma. For more specific results, refine the search by using other search features, such as the location of the trial, the type of treatment, or the name of the drug. General information about clinical trials is available from the NCI Web site.
To Learn More About Childhood Brain Tumors
For more information from the
What You Need to Know About™ Brain Tumors
Pediatric Brain Tumor Consortium (PBTC)
For more childhood
What You Need to Know About™ Cancer
Childhood Cancers
CureSearch for Children's Cancer
Late Effects of Treatment for Childhood Cancer
Adolescents and Young Adults with Cancer
Young People with Cancer: A Handbook for Parents
Care for Children and Adolescents with Cancer
Understanding Cancer Series: Cancer
Cancer Staging
Coping with Cancer: Supportive and Palliative Care
Cancer Library
Information for Survivors/Caregivers/Advocates
Get More Information From NCI
Call 1-800-4-CANCER
For more information, U.S. residents may call the National Cancer Institute's (NCI's) Cancer Information Service toll-free at 1-800-4-CANCER (1-800-422-6237) Monday through Friday from 8:00 a.m. to 8:00 p.m., Eastern Time. A trained Cancer Information Specialist is available to answer your questions.
Chat online
The NCI's LiveHelp® online chat service provides Internet users with the ability to chat online with an Information Specialist. The service is available from 8:00 a.m. to 11:00 p.m. Eastern time, Monday through Friday. Information Specialists can help Internet users find information on NCI Web sites and answer questions about cancer.
Write to us
For more information from the NCI, please write to this address:
NCI Public Inquiries Office
Suite 3036A
6116 Executive Boulevard, MSC8322
Bethesda, MD 20892-8322
Search the NCI Web site
The NCI Web site provides online access to information on cancer, clinical trials, and other Web sites and organizations that offer support and resources for cancer patients and their families. For a quick search, use the search box in the upper right corner of each Web page. The results for a wide range of search terms will include a list of "Best Bets," editorially chosen Web pages that are most closely related to the search term entered.
There are also many other places to get materials and information about cancer treatment and services. Hospitals in your area may have information about local and regional agencies that have information on finances, getting to and from treatment, receiving care at home, and dealing with problems related to cancer treatment.
Find Publications
The NCI has booklets and other materials for patients, health professionals, and the public. These publications discuss types of cancer, methods of cancer treatment, coping with cancer, and clinical trials. Some publications provide information on tests for cancer, cancer causes and prevention, cancer statistics, and NCI research activities. NCI materials on these and other topics may be ordered online or printed directly from the NCI Publications Locator. These materials can also be ordered by telephone from the Cancer Information Service toll-free at 1-800-4-CANCER (1-800-422-6237).
Changes to This Summary (11/04/2011)
The
Changes were made to this summary to match those made to the health professional version.
About PDQ
PDQ is a comprehensive cancer database available on NCI's Web site.
PDQ is the National Cancer Institute's (NCI's) comprehensive cancer information database. Most of the information contained in PDQ is available online at NCI's Web site. PDQ is provided as a service of the NCI. The NCI is part of the National Institutes of Health, the federal government's focal point for biomedical research.
PDQ contains cancer information summaries.
The PDQ database contains summaries of the latest published information on cancer prevention, detection, genetics, treatment, supportive care, and complementary and alternative medicine. Most summaries are available in two versions. The health professional versions provide detailed information written in technical language. The patient versions are written in easy-to-understand, nontechnical language. Both versions provide current and accurate cancer information.
The PDQ cancer information summaries are developed by cancer experts and reviewed regularly.
Editorial Boards made up of experts in oncology and related specialties are responsible for writing and maintaining the cancer information summaries. The summaries are reviewed regularly and changes are made as new information becomes available. The date on each summary ("Date Last Modified") indicates the time of the most recent change.
PDQ also contains information on clinical trials.
A clinical trial is a study to answer a scientific question, such as whether one treatment is better than another. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in order to find new and better ways to help cancer patients. During treatment clinical trials, information is collected about the effects of a new treatment and how well it works. If a clinical trial shows that a new treatment is better than one currently being used, the new treatment may become "standard." In the United States, about two-thirds of children with cancer are treated in a clinical trial at some point in their illness.
Listings of clinical trials are included in PDQ and are available online at NCI's Web site. Descriptions of the trials are available in health professional and patient versions. For additional help in locating a childhood cancer clinical trial, call the Cancer Information Service at 1-800-4-CANCER (1-800-422-6237).
The PDQ database contains listings of groups specializing in clinical trials.
The Children's Oncology Group (COG) is the major group that organizes clinical trials for childhood cancers in the United States. Information about contacting COG is available on the NCI Web site or from the Cancer Information Service at 1-800-4-CANCER (1-800-422-6237).
Connect with us:
Download our App: