Electroencephalogram (EEG) Frequently Asked Questions (FAQ)
Why might a child need an EEG?
A child may need an EEG to look for evidence of, or to get a more specific diagnosis for:
- Seizures and epilepsy
- Abnormal movements
- Changes in behavior
- Loss of developmental milestones
- Sleep disorders that have an unknown cause
- Staring or unresponsive spells
Most EEGs are ordered for children who have unexplained developmental delays or are experiencing symptoms such as loss of consciousness, abnormal movements, or abnormal behavior. An EEG can help determine whether seizures or other brain conditions are causing the symptoms.
Are EEGs safe for children?
Most medical procedures entail some risk, but EEGs, which have been used for almost a century, are very safe. Children who are already prone to have seizures occasionally have them during the test, but the clinical staff is ready to respond immediately if a seizure occurs. The electrodes placed on the skin are passive and only record activity; they do not stimulate the brain, and they present no risk of shock. EEGs do require a child to be still and calm, which can be a challenge, but no part of an EEG hurts.
What are the different types of EEGs?
Outpatient EEGs are the most common type we perform at the Stanford Medicine Children’s Health EEG Lab. They typically take about 90 minutes, during which a child needs to remain still and quiet. A technologist may help the child try to fall asleep at some point during the test and may lead some simple activities, such as a couple of minutes of deep breathing and/or a short period of watching a strobe light. These activities evoke brain wave responses that help with diagnosis.
Ambulatory/home EEGs can help get even more information about a child’s brain while the child goes through daily routines in the comfort of home. Electrodes are pasted on the child’s scalp in the EEG Lab and are attached to a recording device that the child wears in a backpack. Parents are given a switch they can use to electronically mark the EEG recording when they see a seizure or other abnormal events. To get still more information about the relationship between a child’s brain activity and his or her movements, a video camera may be sent home as well. An ambulatory/home EEG typically takes one or two days.
Inpatient EEG
An inpatient is a child who is admitted to and stays over in the hospital while being treated. So, an inpatient EEG is an extended test conducted in the hospital over one or more days. Because the child is under constant and close expert observation, it is possible to get a lot of behavioral data to help interpret the EEG data. If a child has infrequent and/or harder-to-detect seizures, for example, an inpatient EEG may help ensure that a seizure is clearly recorded simultaneously on both video and the EEG so that it can be more precisely diagnosed.
When a patient is admitted for an inpatient EEG, he or she will be made comfortable in a private room and then fitted with electrodes. The child is free to move about the room, watch TV, read, or play video games. Parents stay in the room with their child.
What happens during an EEG?
Parents are welcome to join their children in the EEG room. And children are encouraged to bring a comforting pillow, blanket, or stuffed animal if it will help them feel more relaxed and at home.
During an EEG, the electrical activity of a patient’s brain is plotted on a graph over time and is digitally recorded. For example, an EEG readout looks like this. Depending on what a neurologist is looking for, he or she may record only 10 minutes of sleep or as long as a full night. The image below represents about one minute of EEG readout. Each squiggly horizontal line shows a reading from electrodes in different positions on the child’s scalp:
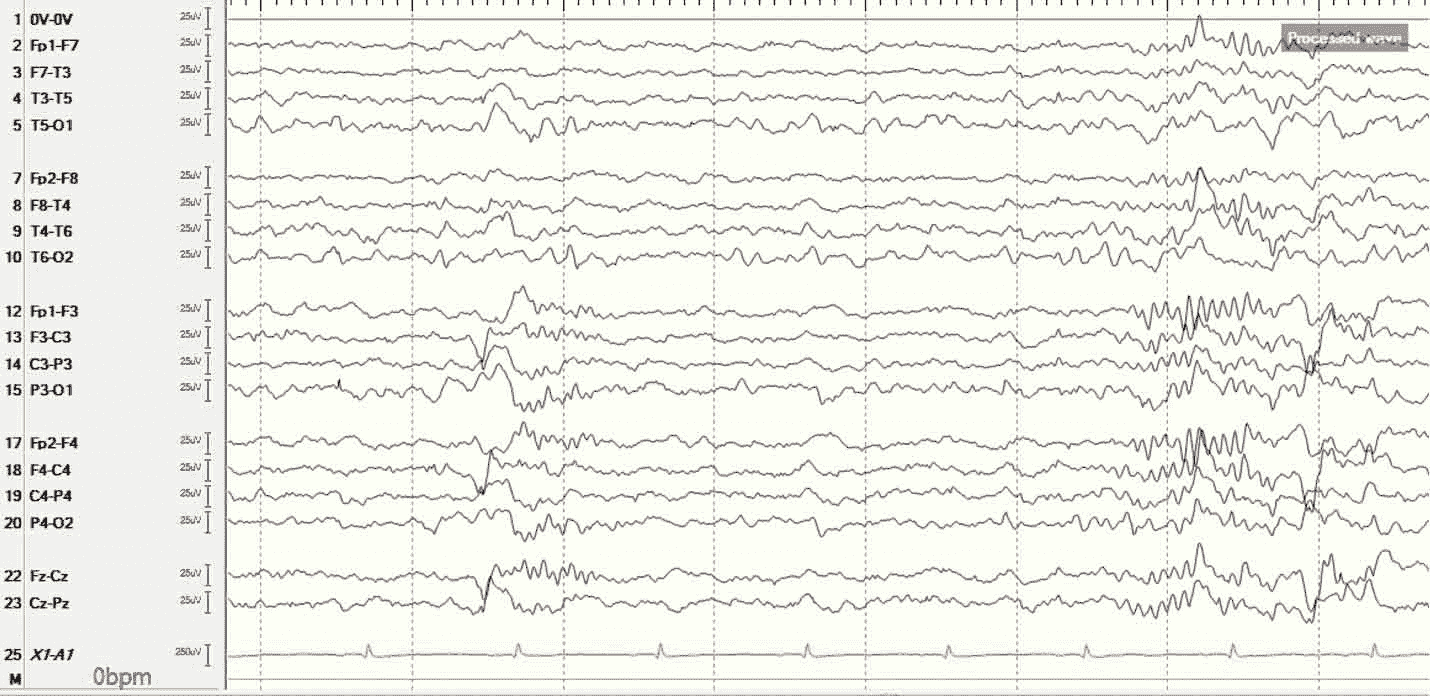 Figure 1. An EEG representing about one minute of a child’s sleep. Each line is a reading from an electrode placed on a different part of the head. Each vertical line represents the passage of eight seconds.
Figure 1. An EEG representing about one minute of a child’s sleep. Each line is a reading from an electrode placed on a different part of the head. Each vertical line represents the passage of eight seconds.
An EEG conducted over the same period of time while a child is awake might look something like this:
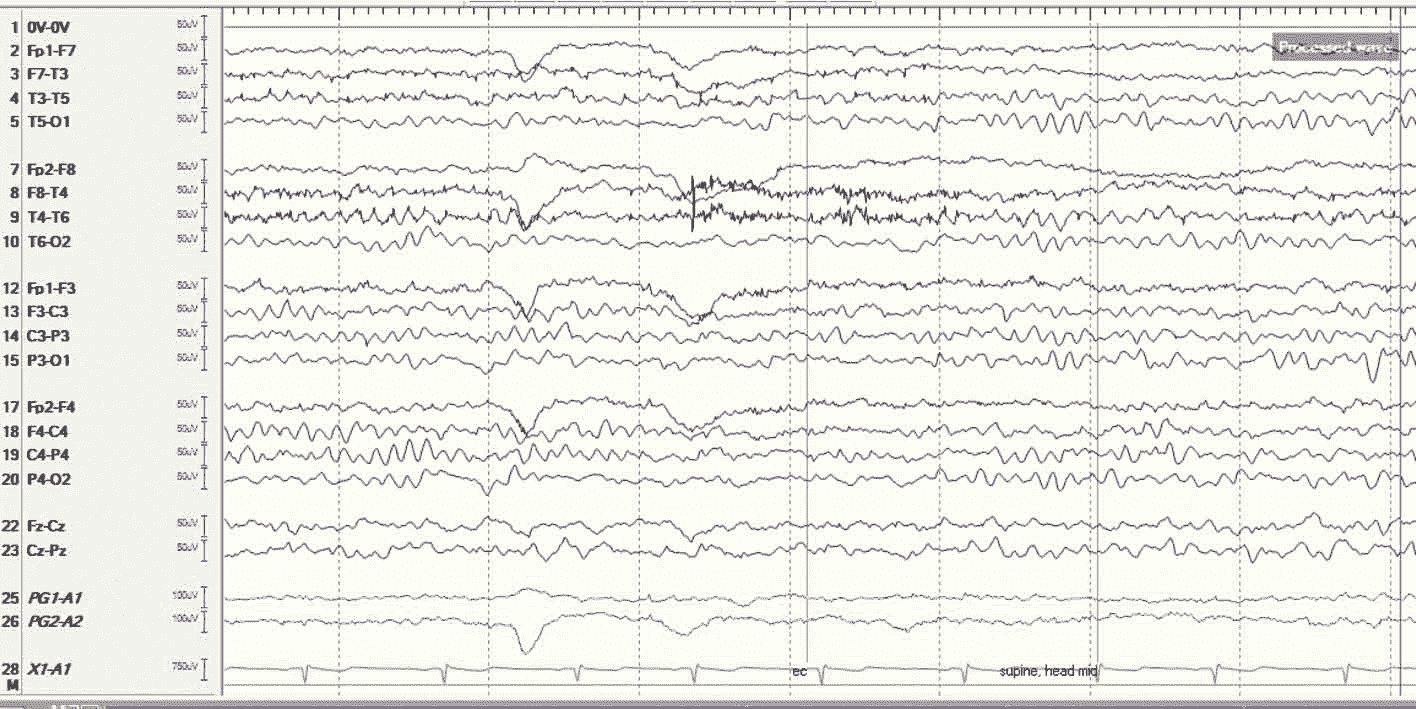 Figure 2. An EEG taken during the same amount of time while the patient is awake. EEGs are packed with information about what is happening in different parts of a child's brain.
Figure 2. An EEG taken during the same amount of time while the patient is awake. EEGs are packed with information about what is happening in different parts of a child's brain.
The EEG technologist may also record video of a child’s physical activity during the test so that it can be matched with the brain wave readings, adding deeper layers of helpful information.
During the test:
- Once a child settles in, the EEG technologist measures his or her head and makes small marks on the scalp with a washable marker. These indicate where stickers holding electrodes are to be placed.
- The technologist cleans each marked area on the scalp with a gritty lotion to ensure that button-sized stickers adhere well to the skin. The technologist attaches the stickers with a sticky paste and then connects a wire (electrode) to each sticker. The wires carry information about the brain’s electrical activity to the EEG recorder.
- When the test begins, the child will be asked to sit or lie as still as possible and sometimes to breathe quickly (hyperventilate), to look at flashing lights, or to try to sleep.
- The test usually takes about 90 minutes.
- A video of the child may also be made during the EEG.
- In rare cases, in a child with a seizure disorder, for example, hyperventilation or flashing lights can cause a seizure to occur during the EEG. If they do, this can give neurologists important information about where in the brain a seizure starts, how it spreads, and what kind of seizure it is.
How do I prepare my child for an EEG?
Preparation for a child’s EEG begins the night before the test.
- The night before an EEG, wash the child’s hair to remove any oil or hair products. So that technologists can properly attach electrodes to the scalp, don’t use hairspray, oil, or gel after washing a child’s hair. Remove any hair extensions, and don’t braid or put hair up; these can interfere with the placement of electrodes.
- A child should not fast before an EEG; low blood sugar can influence the results. Follow all instructions about when a child may eat before having an EEG.
- It is important that a child be sleepy during the test, so do not let him or her drink any caffeinated sodas, coffee, or tea on the day of the EEG and closely follow all instructions about keeping the child awake the night before.
Who performs and reads the EEG?
- An experienced and highly trained team of neurodiagnostic technologists, also called EEG technologists, conduct our EEGs under the supervision of a neurologist. Each technologist is certified by the American Board of Registration of Electroencephalographic and Evoked Potential Technologists (ABRET), an accrediting agency that ensures its members have mastered the latest technologies and the best practices. Just as important is their extensive experience working with children: keeping them happy and relaxed, helping them fall asleep when they need to, and helping them stay awake when they must. technologists also carefully annotate each EEG, identifying normal movements—such as blinking, a yawn, or a sneeze—that may otherwise confound proper interpretation of the test.
- Not only do brain wave patterns change depending on whether a child is asleep or awake, or because of certain neurological abnormalities such as epilepsy, but also they evolve in distinctive ways as a child grows older. That is just one of several important reasons to have a child’s EEG conducted by technologists dedicated to working with children and read by neurologists specializing in pediatric EEG.
What happens after an EEG?
Once the test is complete, the technologist removes the electrodes and washes off the sticky paste with warm water. The child may need a hair washing when back home to remove remnants of the paste. A child may return to his or her normal routine immediately after an EEG.
An epileptologist (a neurologist specializing in the treatment of epilepsy) will read and interpret the EEG and talk to the child’s health care provider about the results. Schedule a follow-up appointment with the child’s health care provider to review the test results. Let him or her know if seizures or other symptoms change or intensify after the test.
Connect with us:
Download our App: