Childhood Non-Hodgkin Lymphoma Treatment (PDQ®)
General Information About Childhood Non-Hodgkin Lymphoma
Childhood non-Hodgkin lymphoma is a disease in which malignant (cancer) cells form in the lymph system.
The
Lymph : Colorless, wateryfluid that travels through the lymph system and carrieswhite blood cells calledlymphocytes . Lymphocytes protect the body againstinfections and the growth oftumors .Lymph vessels : A network of thin tubes that collect lymph from different parts of the body and return it to the bloodstream.Lymph nodes : Small, bean-shaped structures that filter lymph and store white blood cells that help fight infection and disease. Lymph nodes grow along the network of lymph vessels found throughout the body. Clusters of lymph nodes are found in the underarm,pelvis , neck,abdomen , andgroin .Spleen : Anorgan that makes lymphocytes, filters theblood , stores bloodcells , and destroys old blood cells. The spleen is on the left side of the abdomen near thestomach .Thymus : An organ in which lymphocytes grow and multiply. The thymus is in the chest behind the breastbone.Tonsils : Two small masses of lymphtissue at the back of thethroat . The tonsils make lymphocytes.Bone marrow : The soft, spongy tissue in the center of large bones. Bone marrow makes white blood cells,red blood cells , andplatelets .
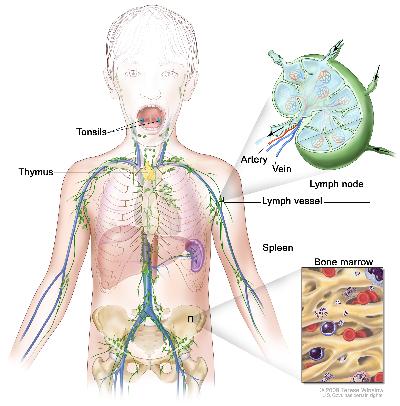
Because lymph tissue is found throughout the body, childhood
Non-Hodgkin lymphoma can occur in both adults and children. Treatment for children is different than treatment for adults. (See the
There are four major types of childhood non-Hodgkin lymphoma.
The specific type of
B-cell non-Hodgkin lymphoma (Burkitt andBurkitt-like lymphoma) andBurkitt leukemia .Diffuse large B-cell lymphoma .Lymphoblastic lymphoma .Anaplastic large cell lymphoma .
There are other types of lymphoma that occur in children. These include the following:
Lymphoproliferative disease associated with a weakened immune system.Rare non-Hodgkin lymphomas that are more common in adults than in children.
Possible signs of childhood non-Hodgkin lymphoma include breathing problems and swollen lymph nodes.
These and other
Trouble breathing.
Wheezing.
Coughing.
High-pitched breathing sounds.
Swelling of the head, neck, upper body or arms.
Trouble swallowing.
Painless swelling of the lymph nodes in the neck, underarm, stomach, or groin.
Fever for no known reason.Weight loss for no known reason.
Night sweats.
Tests that examine the body and lymph system are used to detect (find) and diagnose childhood non-Hodgkin lymphoma.
The following tests and procedures may be used:
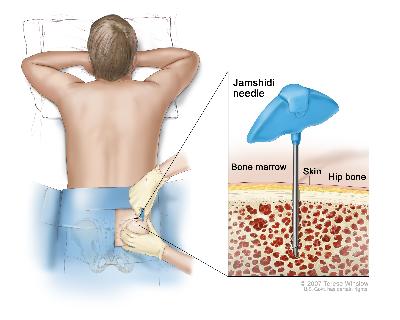
Physical exam and history: An exam of the body to check general signs of health, including checking for signs of disease, such as lumps or anything else that seems unusual. A history of the patient’s health habits and past illnesses and treatments will also be taken.Biopsy : The removal of cells or tissues so they can be viewed under amicroscope by apathologist to check for signs of cancer. One of the following types of biopsies may be done:Excisional biopsy : The removal of an entire lymph node or lump of tissue.Incisional biopsy : The removal of part of a lump, lymph node, or sample of tissue.Core biopsy : The removal of tissue or part of a lymph node using a wide needle.Fine-needle aspiration (FNA) biopsy : The removal of tissue or part of a lymph node using a thin needle.Bone marrow aspiration andbiopsy : The removal of bone marrow, blood, and a small piece of bone by inserting a hollow needle into the hipbone or breastbone.
Immunohistochemistry study : Alaboratory test in which a substance such as anantibody , dye, orradioisotope is added to a sample of cancer tissue to test for certainantigens . This type of study is used to tell the difference between different types of cancer.Cytogenetic analysis: A laboratory test in which cells in a sample of tissue are viewed under a microscope to look for certain changes in thechromosomes .Endoscopy : A procedure to look at organs and tissues inside the body to check forabnormal areas. Anendoscope is inserted through anincision (cut) in the skin or opening in the body, such as the mouth. An endoscope is a thin, tube-like instrument with a light and alens for viewing. It may also have a tool to remove tissue or lymph node samples, which are checked under a microscope for signs of disease.Mediastinoscopy : Asurgical procedure to look at the organs, tissues, and lymph nodes between thelungs for abnormal areas. An incision (cut) is made at the top of thebreastbone and amediastinoscope is inserted into the chest. A mediastinoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove tissue or lymph node samples, which are checked under a microscope for signs of cancer.Anterior mediastinotomy : A surgical procedure to look at the organs and tissues between the lungs and between the breastbone and heart for abnormal areas. An incision (cut) is made next to the breastbone and a mediastinoscope is inserted into the chest. A mediastinoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove tissue or lymph node samples, which are checked under a microscope for signs of cancer. This is also called the Chamberlain procedure.Thoracoscopy : A surgical procedure to look at the organs inside the chest to check for abnormal areas. An incision (cut) is made between two ribs and athoracoscope is inserted into the chest. A thoracoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove tissue or lymph node samples, which are checked under a microscope for signs of cancer. In some cases, this procedure is used to remove part of theesophagus or lung.Thoracentesis : The removal offluid from the space between the lining of the chest and the lung, using a needle. A pathologist views the fluid under a microscope to look for cancer cells.Ultrasound exam: A procedure in which high-energy sound waves (ultrasound) are bounced off internal tissues or organs and make echoes. The echoes form a picture of body tissues called asonogram . The picture can be printed to be looked at later.PET scan (positron emission tomography scan): A procedure to findmalignant tumor cells in the body. A small amount ofradioactive glucose (sugar) isinjected into avein . The PETscanner rotates around the body and makes a picture of where glucose is being used in the body. Malignant tumor cells show up brighter in the picture because they are more active and take up more glucose than normal cells do.Chest x-ray : Anx-ray of the organs and bones inside the chest. An x-ray is a type of energy beam that can go through the body and onto film, making a picture of areas inside the body.CT scan (CAT scan): A procedure that makes a series of detailed pictures of areas inside the body, taken from different angles. The pictures are made by a computer linked to an x-ray machine. Adye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography.
Certain factors affect prognosis (chance of recovery) and treatment options.
The
The age of the child.
The type of lymphoma.
The
stage of the cancer.The number of places outside of the lymph nodes to which the cancer has spread.
Whether the lymphoma has spread to the
central nervous system (brain andspinal cord ).Whether there are certain changes in the chromosomes.
The type of initial treatment.
Whether the lymphoma responds to initial treatment.
The patient’s general health.
Stages of Childhood Non-Hodgkin Lymphoma
After childhood non-Hodgkin lymphoma has been diagnosed, tests are done to find out if cancer cells have spread within the lymph system or to other parts of the body.
The process used to find out if
Physical exam and history: An exam of the body to check general signs of health, including checking for signs of disease, such as lumps or anything else that seems unusual. A history of the patient’s health habits and past illnesses and treatments will also be taken.Complete blood count (CBC): A procedure in which a sample ofblood is drawn and checked for the following:The number of
red blood cells ,white blood cells , andplatelets .The amount of
hemoglobin (theprotein that carriesoxygen ) in the red blood cells.The portion of the sample made up of red blood cells.
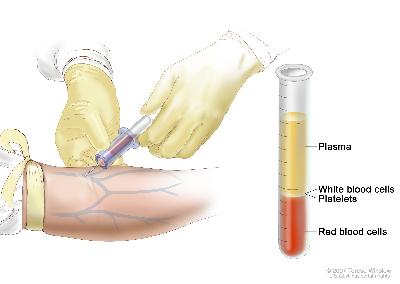 Complete blood count (CBC). Blood is collected by inserting a needle into a vein and allowing the blood to flow into a tube. The blood sample is sent to the laboratory and the red blood cells, white blood cells, and platelets are counted. The CBC is used to test for, diagnose, and monitor many different conditions.
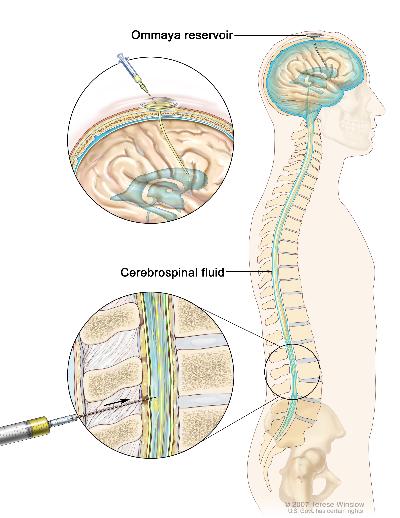
Complete blood count (CBC). Blood is collected by inserting a needle into a vein and allowing the blood to flow into a tube. The blood sample is sent to the laboratory and the red blood cells, white blood cells, and platelets are counted. The CBC is used to test for, diagnose, and monitor many different conditions.Blood chemistry studies : A procedure in which a blood sample is checked to measure the amounts of certain substances released into the blood byorgans andtissues in the body. An unusual (higher or lower than normal) amount of a substance can be a sign of disease in the organ or tissue that makes it.Chest x-ray : Anx-ray of the organs and bones inside the chest. An x-ray is a type of energy beam that can go through the body and onto film, making a picture of areas inside the body.CT scan (CAT scan): A procedure that makes a series of detailed pictures of areas inside the body, taken from different angles. The pictures are made by a computer linked to an x-ray machine. Adye may beinjected into avein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography.Bone marrow aspiration andbiopsy : The removal ofbone marrow , blood, and a small piece of bone by inserting a hollow needle into the hipbone or breastbone. Apathologist views the bone marrow, blood, and bone under a microscope to look for signs of cancer.Lumbar puncture : A procedure used to collectcerebrospinal fluid from thespinal column . This is done by placing a needle into the spinal column. This procedure is also called an LP or spinal tap.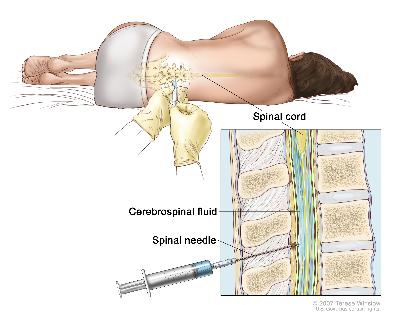 Lumbar puncture. A patient lies in a curled position on a table. After a small area on the lower back is numbed, a spinal needle (a long, thin needle) is inserted into the lower part of the spinal column to remove cerebrospinal fluid (CSF, shown in blue). The fluid may be sent to a laboratory for testing.
Lumbar puncture. A patient lies in a curled position on a table. After a small area on the lower back is numbed, a spinal needle (a long, thin needle) is inserted into the lower part of the spinal column to remove cerebrospinal fluid (CSF, shown in blue). The fluid may be sent to a laboratory for testing.Bone scan : A procedure to check if there are rapidly dividing cells, such as cancer cells, in the bone. A very small amount of radioactive material is injected into a vein and travels through the bloodstream. The radioactive material collects in the bones and is detected by a scanner.MRI (magnetic resonance imaging): A procedure that uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body. This procedure is also called nuclear magnetic resonance imaging (NMRI).Endoscopy : A procedure to look at organs and tissues inside the body to check for abnormal areas. Anendoscope is inserted through anincision (cut) in the skin or opening in the body, such as the mouth. An endoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove tissue orlymph node samples, which are checked under a microscope for signs of disease.
There are three ways that cancer spreads in the body.
The three ways that cancer spreads in the body are:
Through
tissue . Cancerinvades the surrounding normal tissue.Through the
lymph system . Cancer invades the lymph system and travels through thelymph vessels to other places in the body.Through the
blood . Cancer invades theveins andcapillaries and travels through the blood to other places in the body.
When cancer
The following stages are used for childhood non-Hodgkin lymphoma:
Stage I
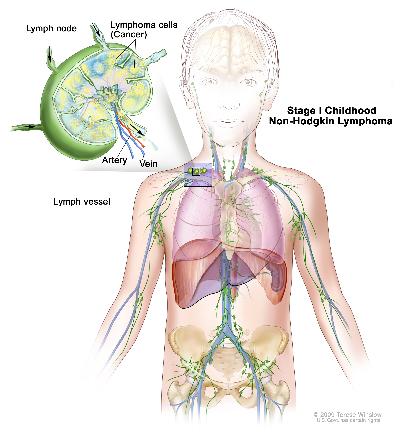
In
in one group of
lymph nodes ; orin one area outside the lymph nodes.
No cancer is found in the
Stage II
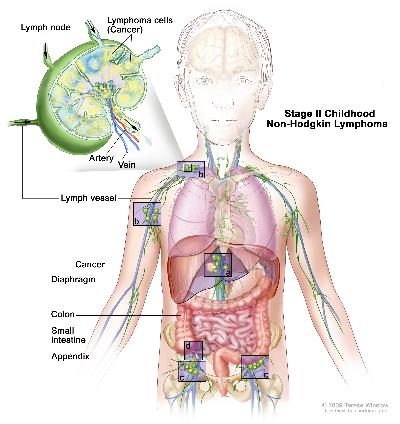
In
in one area outside the
lymph nodes and in nearby lymph nodes; orin two or more areas above or below the
diaphragm , and may or may not have spread to nearby lymph nodes; orto have started in the
stomach orintestines and can be completely removed bysurgery . Cancer may or may not have spread to certain nearby lymph nodes.
Stage III
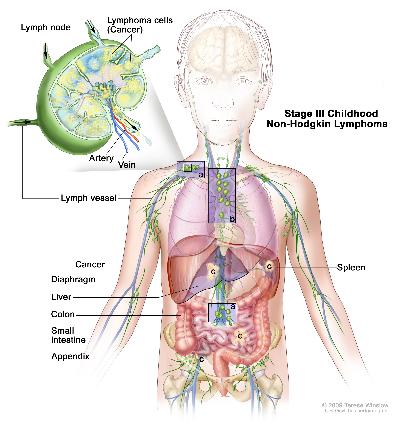
In
in at least one area above the
diaphragm and in at least one area below the diaphragm; orto have started in the chest; or
to have started in the
abdomen and spread throughout the abdomen, and cannot be completely removed bysurgery ; orin the area around the
spine .
Stage IV
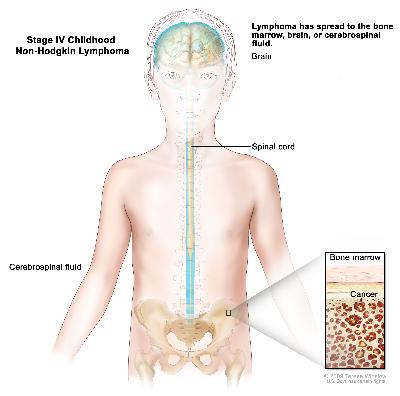
In
Childhood non-Hodgkin lymphoma is also described as low-stage or high-stage.
Treatment for childhood
Recurrent Childhood Non-Hodgkin Lymphoma
Treatment Option Overview
There are different types of treatment for children with non-Hodgkin lymphoma.
Different types of treatment are available for children with
Because cancer in children is rare, taking part in a clinical trial should be considered. Some clinical trials are open only to patients who have not started treatment.
Children with non-Hodgkin lymphoma should have their treatment planned by a team of doctors with expertise in treating childhood cancer.
Treatment will be overseen by a
Radiation oncologist .Pediatric hematologist .Pediatric surgeon .Pediatric nurse specialist .Rehabilitation specialist .Psychologist .Social worker .
Some cancer treatments cause side effects months or years after treatment has ended.
Physical problems.
Changes in mood, feelings, thinking, learning, or memory.
Second cancers (new types of cancer).
Some late effects may be treated or controlled. It is important to talk with your child's doctors about the effects cancer treatment can have on your child. (See the
Four types of standard treatment are used:
Chemotherapy
See Drugs Approved for Non-Hodgkin Lymphoma for more information.
Radiation therapy (in certain patients)
High-dose chemotherapy with stem cell transplant
This treatment is a way of giving
See Drugs Approved for Non-Hodgkin Lymphoma for more information.
Targeted therapy
Monoclonal antibody
Tyrosine kinase inhibitors (TKIs) block signals that tumors need to grow. Some TKIs also keep tumors from growing by preventing the growth of new
See Drugs Approved for Non-Hodgkin Lymphoma for more information.
New types of treatment are being tested in clinical trials.
Information about clinical trials is available from the NCI Web site.
Patients may want to think about taking part in a clinical trial.
For some patients, taking part in a
Many of today's standard treatments for cancer are based on earlier clinical trials. Patients who take part in a clinical trial may receive the standard treatment or be among the first to receive a new treatment.
Patients who take part in clinical trials also help improve the way cancer will be treated in the future. Even when clinical trials do not lead to effective new treatments, they often answer important questions and help move research forward.
Patients can enter clinical trials before, during, or after starting their cancer treatment.
Some clinical trials only include patients who have not yet received treatment. Other trials test treatments for patients whose cancer has not gotten better. There are also clinical trials that test new ways to stop cancer from
Clinical trials are taking place in many parts of the country. See the Treatment Options section that follows for links to current treatment clinical trials. These have been retrieved from
Follow-up tests may be needed.
Some of the tests that were done to
Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your condition has changed or if the cancer has
Treatment Options for Childhood Non-Hodgkin Lymphoma
A link to a list of current
Low-stage Childhood Non-Hodgkin Lymphoma
New treatments are being studied in
Check for U.S. clinical trials from NCI's list of cancer clinical trials that are now accepting patients with stage I childhood large cell lymphoma, stage I childhood small noncleaved cell lymphoma, stage I childhood lymphoblastic lymphoma, stage I childhood anaplastic large cell lymphoma, stage II childhood large cell lymphoma, stage II childhood small noncleaved cell lymphoma, stage II childhood lymphoblastic lymphoma and stage II childhood anaplastic large cell lymphoma. For more specific results, refine the search by using other search features, such as the location of the trial, the type of treatment, or the name of the drug. General information about clinical trials is available from the NCI Web site.
High-stage Childhood B-cell Non-Hodgkin Lymphoma
Check for U.S. clinical trials from NCI's list of cancer clinical trials that are now accepting patients with stage III childhood large cell lymphoma, stage III childhood small noncleaved cell lymphoma, stage IV childhood large cell lymphoma and stage IV childhood small noncleaved cell lymphoma. For more specific results, refine the search by using other search features, such as the location of the trial, the type of treatment, or the name of the drug. General information about clinical trials is available from the NCI Web site.
High-stage Childhood Lymphoblastic Lymphoma
Check for U.S. clinical trials from NCI's list of cancer clinical trials that are now accepting patients with stage III childhood lymphoblastic lymphoma and stage IV childhood lymphoblastic lymphoma. For more specific results, refine the search by using other search features, such as the location of the trial, the type of treatment, or the name of the drug. General information about clinical trials is available from the NCI Web site.
High-stage Childhood Anaplastic Large-cell Lymphoma
New combinations of
Check for U.S. clinical trials from NCI's list of cancer clinical trials that are now accepting patients with stage III childhood anaplastic large cell lymphoma and stage IV childhood anaplastic large cell lymphoma. For more specific results, refine the search by using other search features, such as the location of the trial, the type of treatment, or the name of the drug. General information about clinical trials is available from the NCI Web site.
Recurrent Childhood Non-Hodgkin Lymphoma
There is no
All patients with recurrent childhood non-Hodgkin lymphoma should be considered for
Burkitt lymphoma and diffuse large B-cell lymphoma
Treatment options for recurrent
Combination chemotherapy .Combination chemotherapy and
targeted therapy with amonoclonal antibody .High-dose chemotherapy withstem cell transplant .
Lymphoblastic lymphoma
Treatment options for recurrent
Combination chemotherapy.
High-dose chemotherapy with stem cell transplant.
Anaplastic large-cell lymphoma
Treatment options for recurrent
Chemotherapy with one or moredrugs .High-dose chemotherapy with stem cell transplant.
A clinical trial of
targeted therapy with atyrosine kinase inhibitor .
Check for U.S. clinical trials from NCI's list of cancer clinical trials that are now accepting patients with recurrent childhood non-Hodgkin lymphoma. For more specific results, refine the search by using other search features, such as the location of the trial, the type of treatment, or the name of the drug. General information about clinical trials is available from the NCI Web site.
Lymphoproliferative Disease Associated with a Weakened Immune System
Surgery with or withoutradiation therapy .Combination chemotherapy .Low-dose
chemotherapy .
One of the treatments being studied in
To Learn More About Childhood Non-Hodgkin Lymphoma
For more information from the
What You Need to Know About™ Non-Hodgkin Lymphoma
Drugs Approved for Non-Hodgkin Lymphoma
Understanding Cancer Series: Blood Stem Cell Transplants
Bone Marrow Transplantation and Peripheral Blood Stem Cell Transplantation
Targeted Cancer Therapies
Understanding Cancer Series: Targeted Therapies (Advances in Targeted Therapies and Targeted Therapies for Lymphoma)
Understanding Cancer Series: The Immune System
For more childhood
What You Need to Know About™ Cancer
Childhood Cancers
CureSearch for Children's Cancer
Late Effects of Treatment for Childhood Cancer
Adolescents and Young Adults with Cancer
Young People with Cancer: A Handbook for Parents
Care for Children and Adolescents with Cancer
Understanding Cancer Series: Cancer
Cancer Staging
Coping with Cancer: Supportive and Palliative Care
Cancer Library
Information for Survivors/Caregivers/Advocates
Get More Information From NCI
Call 1-800-4-CANCER
For more information, U.S. residents may call the National Cancer Institute's (NCI's) Cancer Information Service toll-free at 1-800-4-CANCER (1-800-422-6237) Monday through Friday from 8:00 a.m. to 8:00 p.m., Eastern Time. A trained Cancer Information Specialist is available to answer your questions.
Chat online
The NCI's LiveHelp® online chat service provides Internet users with the ability to chat online with an Information Specialist. The service is available from 8:00 a.m. to 11:00 p.m. Eastern time, Monday through Friday. Information Specialists can help Internet users find information on NCI Web sites and answer questions about cancer.
Write to us
For more information from the NCI, please write to this address:
NCI Public Inquiries Office
Suite 3036A
6116 Executive Boulevard, MSC8322
Bethesda, MD 20892-8322
Search the NCI Web site
The NCI Web site provides online access to information on cancer, clinical trials, and other Web sites and organizations that offer support and resources for cancer patients and their families. For a quick search, use the search box in the upper right corner of each Web page. The results for a wide range of search terms will include a list of "Best Bets," editorially chosen Web pages that are most closely related to the search term entered.
There are also many other places to get materials and information about cancer treatment and services. Hospitals in your area may have information about local and regional agencies that have information on finances, getting to and from treatment, receiving care at home, and dealing with problems related to cancer treatment.
Find Publications
The NCI has booklets and other materials for patients, health professionals, and the public. These publications discuss types of cancer, methods of cancer treatment, coping with cancer, and clinical trials. Some publications provide information on tests for cancer, cancer causes and prevention, cancer statistics, and NCI research activities. NCI materials on these and other topics may be ordered online or printed directly from the NCI Publications Locator. These materials can also be ordered by telephone from the Cancer Information Service toll-free at 1-800-4-CANCER (1-800-422-6237).
Changes to This Summary (11/07/2011)
The
Changes were made to this summary to match those made to the health professional version.
About PDQ
PDQ is a comprehensive cancer database available on NCI's Web site.
PDQ is the National Cancer Institute's (NCI's) comprehensive cancer information database. Most of the information contained in PDQ is available online at NCI's Web site. PDQ is provided as a service of the NCI. The NCI is part of the National Institutes of Health, the federal government's focal point for biomedical research.
PDQ contains cancer information summaries.
The PDQ database contains summaries of the latest published information on cancer prevention, detection, genetics, treatment, supportive care, and complementary and alternative medicine. Most summaries are available in two versions. The health professional versions provide detailed information written in technical language. The patient versions are written in easy-to-understand, nontechnical language. Both versions provide current and accurate cancer information.
The PDQ cancer information summaries are developed by cancer experts and reviewed regularly.
Editorial Boards made up of experts in oncology and related specialties are responsible for writing and maintaining the cancer information summaries. The summaries are reviewed regularly and changes are made as new information becomes available. The date on each summary ("Date Last Modified") indicates the time of the most recent change.
PDQ also contains information on clinical trials.
A clinical trial is a study to answer a scientific question, such as whether one treatment is better than another. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in order to find new and better ways to help cancer patients. During treatment clinical trials, information is collected about the effects of a new treatment and how well it works. If a clinical trial shows that a new treatment is better than one currently being used, the new treatment may become "standard." In the United States, about two-thirds of children with cancer are treated in a clinical trial at some point in their illness.
Listings of clinical trials are included in PDQ and are available online at NCI's Web site. Descriptions of the trials are available in health professional and patient versions. For additional help in locating a childhood cancer clinical trial, call the Cancer Information Service at 1-800-4-CANCER (1-800-422-6237).
The PDQ database contains listings of groups specializing in clinical trials.
The Children's Oncology Group (COG) is the major group that organizes clinical trials for childhood cancers in the United States. Information about contacting COG is available on the NCI Web site or from the Cancer Information Service at 1-800-4-CANCER (1-800-422-6237).



Connect with us:
Download our App: