Contact us
If you would like to learn more or if you are ready to make an appointment, please call our team.
Notice of West building lobby closure at Lucile Packard Children’s Hospital Stanford
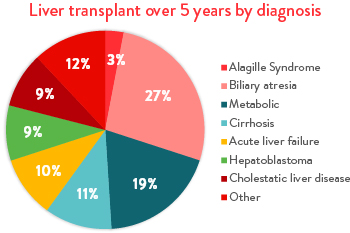
The liver is a vital organ in the body, one we can’t live without. A liver transplant replaces your child’s diseased liver with a healthy liver. Liver transplant is the best option when other treatments stop working. Over the past five years, biliary atresia, metabolic liver disease, liver cirrhosis, acute liver failure, and hepatoblastoma account for more than 75% of transplants performed.
By offering several types of transplants beyond the traditional whole liver transplant, we increase the pool of donor organs available, advocate with the review board to move your child up the list, and bring your child to transplant quickly to create the best possible outcome for your child.
We are proud to be a national leader in performing successful ABOi liver transplants.
Finding a matching liver donor can be difficult. You’ve likely heard about long waiting lists for donor organs. This innovative technique closes the gap between the number of donor organs available and the number of children who need them, saving lives.
In recent years, great progress has been made with ABO incompatible (ABOi) liver transplants. Today, rejection is limited by using current techniques and medications to suppress your child’s immune system so that it doesn’t see the new liver as foreign tissue.
ABO incompatible liver transplants make it possible for parents and family members who are not a full match to become donors.
Living donor liver transplant (LDLT) saves lives by expanding the number of organs available for transplant and shortening wait times. Our liver transplant program is one of a handful of transplant centers in the nation to offer adult-to-child living donor transplantation. We’re pleased to offer an innovative, leading-edge living donor option called 3-D laparoscopic hepatectomy. This minimally invasive procedure reduces operating time and may mean a faster recovery.
In this procedure, a healthy, living adult donates a portion of his or her liver to your critically ill child. In both the donor and the recipient, the remaining tissue grows into a fully functioning liver within six to eight weeks. Your child’s new liver will continue to grow throughout life.
Potential donors include parents, aunts, uncles, extended family, and even close family friends. Donors are tested for compatibility and need active insurance and a primary care physician. For more information about the living donor program, please contact the Living Donor Coordinator at (650) 724-5672 or visit Stanford Health Care’s Living Donor page.
Becoming a donor is immensely impactful and saves the life of a child. If you would like to pursue becoming a donor, please complete the online questionnaire to start the process and learn more. The questionnaire takes an average of 15 minutes to complete and must be completed in one sitting. |
Lucile Packard Children’s Hospital Stanford is known for its high-performing Pediatric Transplant Center, which is a national pediatric organ transplant volume leader. We offer a full range of pediatric transplants, including liver, kidney, intestinal, heart, and lung transplants.
We’ve mastered multidisciplinary care, bringing pediatric specialists (cardiology, nephrology, pulmonology, etc.) and pediatric subspecialists (fetal cardiology, PACT, PICU, etc.) together to customize your child’s care team, with your family at the center. We work closely with all of the hospital’s transplant programs to provide combined solid organ transplants. We perform combined liver-kidney, liver-intestine, heart-liver, and liver-lung transplants as well as some rare heart-liver-kidney and heart-lung-kidney transplants.
There are several childhood diseases that require heart-liver transplants, including congenital heart disease. Lung-liver multiorgan transplants can be needed in children with cystic fibrosis, and liver-kidney transplants can be required for children with advanced metabolic kidney or liver disease. Children with intestinal failure requiring transplant sometimes also need a new liver.
While waiting for transplant, we set your child up for success by increasing his or her overall health with such methods as nutrition and dialysis, making sure that he or she is healthy and stable before transplant.
Connect with us:
Download our App: