Multiple Sclerosis and Pregnancy
What is multiple sclerosis?
Multiple sclerosis (MS) is a chronic disease of the central nervous system, which is made up of the brain and spinal cord. MS is unpredictable. The symptoms of MS can range from mild to disabling, such as losing the ability to write, speak, or walk.
What causes multiple sclerosis?
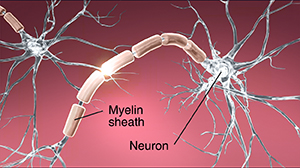
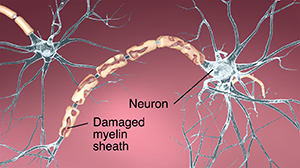
The cause of MS is unknown. Many things may contribute to someone getting MS, including viruses, autoimmune disorders, environmental factors, and genetic factors. But all of the possible causes share a common feature. The body's immune system attacks its own nervous tissue. In MS, the immune system attacks the layer of protein and fatty substance called myelin that surrounds and protects the nerve fibers in the central nervous system. Myelin insulates the electrical signals the nervous system uses to communicate. When this insulation is destroyed, communication is interrupted. Parts of the nervous system become permanently damaged.
What are the symptoms of multiple sclerosis?
Symptoms of MS are erratic. They may be mild or severe. They may last a short or long time. They may appear in various combinations, depending on the part of the nervous system affected. Throughout the course of the illness, you may have any or all of these symptoms:
Muscle weakness in the arms and legs
Trouble with coordination
Impaired walking or standing
Partial or complete paralysis
Spasticity (involuntary increased tone of muscles leading to stiffness and spasms)
Fatigue (may be triggered by physical activity, may ease with rest, or may be constant and persistent)
Loss of sensation or tingling or numbness
Speech problems
Tremor
Dizziness
Hearing loss
Loss of vision or changes in vision
Loss of bowel and bladder control
Sexual dysfunction
Pain
Emotional changes
Changes in reflexes
MS may also cause cognitive effects. The effects may be mild. They're often found only after thorough testing. They may include problems with:
Concentration
Attention
Memory
Judgment
The symptoms of MS may look like other health problems. Always see your healthcare provider for a diagnosis.
How is multiple sclerosis diagnosed?
Your healthcare provider will do a thorough medical history and a physical exam as the first steps toward diagnosis of MS. You'll be asked about all of your symptoms, how often they occur and how long they last.
You'll likely have an MRI. This test can find the unique scars in the central nervous system.
In some cases, you may need lab tests or a lumbar puncture to confirm the diagnosis.
How is multiple sclerosis treated?
There is no known cure for MS. But there are disease-modifying therapies available that can slow the progression of the disease and improve symptoms. These include:
Beta-interferons
Glatiramer acetate
Monoclonal antibodies
Dimethyl fumarate
Fingolimod
Teriflunomide
There are also treatments to help manage symptoms, treat flare-ups or relapses, improve your function and safety, and provide much needed emotional support. The following rehabilitation therapies may also help:
Physical therapy
Occupational therapy
Speech therapy and swallowing assistance
Cognitive therapy
Assistive devices, like splints
Living with multiple sclerosis while pregnant
Pregnancy doesn't appear to speed up the course or worsen the effects of MS. Several studies suggest that MS is less likely to flare up late in pregnancy. There may be a slightly higher risk for a flare-up or relapse right after pregnancy. Talk with your healthcare provider about any concerns you have.
The disabling effects of the disease may make it physically hard to carry a pregnancy. Muscle weakness and coordination problems may increase the likelihood for falls. Fatigue may get worse. Wheelchair dependence may increase the risk for urinary tract infections. There is no evidence that MS causes infertility. Studies have shown that pregnancy, delivery, and rate of birth defects aren't majorly different in women with MS compared with those without MS.
Many of the medicines used to treat MS may have adverse effects on a fetus. It's important to talk with your healthcare provider if you're thinking about pregnancy or if you become pregnant. Your provider will discuss the risks and benefits of the various medicines with you, including any possible effects on your baby and your MS.
During pregnancy, you'll need close monitoring to keep track of the disease and the health of the fetus. You may need more frequent prenatal visits. If you have an MS flare-up, you may be given medicines, such as steroids, which are only considered safe in the second and third trimester. Talk with your provider for more information.
Supportive treatment and rehabilitation for MS are especially important during pregnancy. Rehab varies depending on your symptoms. But it may help with the following:
Doing normal activities of daily living (ADLs)
Maintaining independence
Getting family involved
Using assistive devices (for example, canes, braces, and walkers)
Setting an appropriate exercise program to promote muscle strength, endurance, and control
Re-establishing motor skills
Improving communication skills if you have trouble speaking because of weakness or lack of coordination of face and tongue muscles
Managing bowel or bladder incontinence
Providing cognitive retraining
Adapting the home environment for safety and usability
During labor, you may not have pelvic sensation and not feel pain with contractions. This may also make it hard to tell when labor starts. Delivery of the baby may be harder if you have MS. While labor itself isn't affected, MS can affect the muscles and nerves needed for pushing. For this reason, you may need a cesarean section or delivery with the help of forceps or vacuum.
After childbirth, breastfeeding may reduce the risk of an MS flare-up. Talk with your provider about whether disease modifying medicines may be used when breastfeeding.
When should I call my healthcare provider?
Call your healthcare provider if you have several of the classic symptoms of MS so that treatment can begin right away.
If you have MS and want to get pregnant, discuss the benefits and risks of a pregnancy with your MS specialist before becoming pregnant.
If you're pregnant and have MS, tell your provider as soon as possible.
Key points about multiple sclerosis during pregnancy
There is no cure for MS. But there are many ways to help slow the progression of the disease and manage symptoms.
With MS, you may have long periods of remission of your symptoms.
Pregnancy isn't ruled out just because you have MS. Pregnancy doesn't seem to speed up or make MS worse.
MS can make carrying a pregnancy harder. It may also make labor and delivery harder.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
Know the reason for your visit and what you want to happen.
Before your visit, write down questions you want answered.
Bring someone with you to help you ask questions and remember what your provider tells you.
At the visit, write down the name of a new diagnosis and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are and when they should be reported.
Ask if your condition can be treated in other ways.
Know why a test or procedure is recommended and what the results could mean.
Know what to expect if you don't take the medicine or have the test or procedure.
If you have a follow-up appointment, write down the date, time, and purpose for that visit.
Know how you can contact your healthcare provider if you have questions.
Connect with us:
Download our App: