Oral and Oropharyngeal Cancers
What are oral and oropharyngeal cancers?
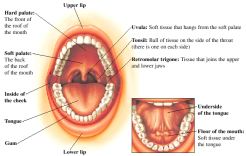
Oral cancer is cancer found in the oral cavity (the mouth area). Oropharyngeal cancer is cancer found in the oropharynx (the throat area at the back of the mouth).
Oral cavity and oropharyngeal cancers will be diagnosed in 36,000 U.S. adults in 2013, according to the American Cancer Society (ACS).
The oral cavity includes:
The lips, teeth, and gums
The front two-thirds of the tongue
The lining inside the lips and cheeks (buccal mucosa)
The floor of the mouth (under the tongue)
The top of the mouth (hard palate)
The small area behind the wisdom teeth
The oropharynx includes:
The back one-third of the tongue
The soft palate
The tonsils
The back of the throat
What causes oral and oropharyngeal cancers?
The main causes of are:
Tobacco use
Alcohol use
Other causes may include the following:
A diet low in fruits and vegetables
Human papillomavirus (HPV) infection
Excessive sun exposure, which, like elsewhere on the body, can cause cancer on the lip
What are the symptoms of oral and oropharyngeal cancers?
The following are the most common symptoms. However, each individual may experience symptoms differently. Symptoms may include:
A lip or mouth sore that does not heal
A white or red patch on the gums, tongue, or lining of mouth
A lump on the lip or in the mouth or throat
Unusual bleeding, pain, or numbness in the mouth area
Swelling of the jaw or neck
Pain in the ear
Change in voice
A chronic sore throat
Feeling as if something is caught in the throat
Pain or difficulty in swallowing or chewing
Cough
The symptoms of oral and oropharyngeal cancers may resemble other disorders or medical problems. Always consult your health care provider for a diagnosis.
What are the different types of oral and oropharyngeal cancers?
Tumors can develop anywhere in the oral cavity and oropharynx (or the back of the mouth where it connects with the throat). Some tumors are benign (noncancerous), some may be precancerous (a condition that may become cancerous), while others may be cancerous. Different types of cancer may develop in different areas of the mouth and throat.
What are benign tumors?
Many forms of benign (noncancerous) tumors can appear in the oral cavity or oropharynx (in addition to other sites in/on the body), including:
Condyloma acuminatum (also known as genital warts) |
A small, moist, pink or red growth that grows alone or in cauliflower-like clusters |
|---|---|
Eosinophilic granuloma |
A benign tumor which most often affects children and adolescents and is usually found in a bone or the lungs |
Fibroma |
A benign tumor consisting of fibrous connective tissues |
Keratoacanthoma |
A flesh-colored, fast-growing bump on the skin with a keratin plug in the center (keratin, the main component of the external layer of skin, hair, and nails, is a tough substance) |
Leiomyoma |
A tumor of the smooth muscle, often found in the esophagus, small intestine, uterus, or stomach |
Lipoma |
A tumor made up of mature fat cells |
Neurofibroma |
A fibrous tumor consisting of nerve tissue |
Odontogenic tumors |
Tumors in the jaw that start in the tooth-forming tissues |
Osteochondroma |
A tumor made up of bone and cartilage |
Papilloma |
A tumor that resembles a wart, growing on the epithelium (the cells that form the skin and mucous membranes) |
Pyogenic granuloma |
A small, round bump that often has an ulcerated surface |
Rhabdomyoma |
A striated-muscle tumor that may appear on the tongue, pharynx, uterus, vagina, or heart |
Schwannoma |
A single tumor that grows in the neurilemma (Schwann's sheath) of nerves |
Verruciform xanthoma |
Wart-shaped tumors |
Some benign tumors disappear on their own. Others may have to be removed surgically. Most benign tumors do not recur (come back). Always consult your health care provider for a diagnosis.
What oral conditions may be precancerous?
Two conditions in the mouth — leukoplakia and erythroplakia — actually can be precursors to cancer. Often caused by smoking or chewing tobacco, these (initially) benign conditions can occur anywhere in the mouth. Only a biopsy can determine whether precancerous cells (dysplasia) or cancer cells are present in a leukoplakia or erythroplakia.
Leukoplakia. A condition characterized by a whitish patch that develops inside the mouth or throat.
Erythroplakia. A condition characterized by a red, raised patch that develops inside the mouth.
Treatment for leukoplakias or erythroplakias may include use of retinoids — medications that are related to vitamin A — to eliminate, reduce, and/or prevent dysplasia from forming.
What are malignant tumors?
Although there are several types of malignant oral and oropharyngeal cancers, more than 90% of all diagnosed oral and oropharyngeal cancers are squamous cell carcinoma.
Squamous cell carcinoma |
Also known as squamous cell cancer, this type of cancer originates in the squamous cell layer in the lining of the oral cavity and oropharynx. In the early stages, this cancer is present only in the lining layer of cells (called carcinoma in situ). When the cancer spreads beyond the lining, it is called invasive squamous cell cancer. |
|---|---|
Verrucous carcinoma |
Although also considered a type of squamous cell carcinoma, this low-grade cancer rarely metastasizes (spreads to distant sites). Comprising less than 5% of all diagnosed oral cancers, verrucous carcinoma can spread deeply into surrounding tissue, requiring surgical removal with a wide margin of surrounding tissue. |
Minor salivary gland cancers |
The lining of the oral cavity and oropharynx contains numerous salivary glands. Sometimes cancer will originate in a salivary gland. Treatment depends on the type and location of the salivary gland cancer, as well as the extent of spreading. According to the ACS, salivary gland cancers are rare. |
What is a risk factor?
A risk factor is anything that may increase a person's chance of developing a disease. It may be an activity, such as smoking, diet, family history, or many other things. Different diseases, including cancers, have different risk factors.
Although these factors can increase a person's risk, they do not necessarily cause the disease. Some people with one or more risk factors never develop the disease, while others develop disease and have no known risk factors.
But, knowing your risk factors to any disease can help to guide you into the appropriate actions, including changing behaviors and being clinically monitored for the disease.
What are the risk factors for oral and oropharyngeal cancers?
Although heredity also plays a factor, certain lifestyle habits and health conditions can increase a person's risk for developing oral and oropharyngeal cancers. These include, but are not limited to:
Tobacco use |
The majority of patients with oral and oropharyngeal cancers use tobacco in one form or another. Tobacco can damage cells in the lining of the oral cavity and oropharynx, causing abnormal cells to grow more rapidly to repair the damage. Researchers believe that the DNA-damaging chemicals in tobacco are linked to the increased risk of oral and oropharyngeal cancers, according to the ACS. |
|---|---|
Alcohol use |
The majority of patients with oral and oropharyngeal cancers use alcohol frequently. Paired with tobacco use, patients who drink and smoke increase their risk of developing oral and oropharyngeal cancers even more. Researchers have found that alcohol increases the penetration of DNA-damaging chemicals in the lining of the oral cavity and oropharynx, according to the ACS. |
Sunlight |
Prolonged exposure to ultraviolet radiation from the sun can cause skin cancer. People who are outdoors for an extended period of time increase their risk of lip cancer, as well. |
Chronic irritation |
Chronic irritation to the lining of the mouth, due to poorly fitting dentures or other reasons, may increase a person's risk for oral cancer. |
Lack of fruits and vegetables in diet |
Research has suggested that fruits and vegetables, which contain antioxidants that can "trap" harmful molecules, can decrease the risk for oral and oropharyngeal cancers (and other cancers). Thus, it is speculated that persons with a low intake of these types of foods are at an increased risk for (oral and oropharyngeal) cancer. |
Human papillomavirus (HPV) infection |
HPV usually causes warts and has been linked to cervical, vaginal, and penile cancers. HPV also increases the risk for cancers of the oral cavity and oropharynx. |
Males |
Oral and oropharyngeal cancers are twice as common in men then in women, partly because men are more likely to use tobacco and alcohol. |
Can oral and oropharyngeal cancers be prevented?
It is important to detect cancers of the oral cavity and oropharynx as early as possible because treatment works best before the disease has spread. The National Cancer Institute (NCI) and ACS encourage people to take an active role in the early detection of these cancers by performing monthly self-examinations. The Oral Health Education Foundation recommends the following steps (below) when examining your mouth. Take special note of any red or white patches, lumps or thickening of skin, tissue, or gums, a sore that either does not heal properly (after a 1- to 2-week period), or a sore that tends to bleed easily or excessively. In addition, be sure to take note of a persistent sore throat, hoarseness, or difficulty maneuvering the jaw during chewing or swallowing. Be sure to consult your doctor right away if any of these symptoms are present:
Remove any dental products in the mouth.
Visually look and touch your mouth, including the lips and gums.
Check the roof of your mouth.
Check the inside of the cheeks and the back gums.
Check the tongue, including the sides and underneath.
Check for enlarged lymph nodes in the neck and under the jaw.
Regular dental checkups that include an examination of the entire mouth are also important in the early detection of oral and oropharyngeal cancers or precancerous conditions. Your doctor should also check your mouth as part of a routine physical exam.
How are oral and oropharyngeal cancers diagnosed?
In addition to a complete medical history and physical examination, diagnostic procedures for oral cancers of the oral cavity and oropharynx may include one or more of the following:
Biopsy. A procedure in which tissue samples are removed (with a needle or during surgery) from the body for examination under a microscope to determine if cancer or other abnormal cells are present.
Computed tomography (CT or CAT scan). A noninvasive procedure that takes horizontal, or axial, images of the brain or other internal organs to detect any abnormalities that may not show up on an ordinary X-ray.
Ultrasonography. A diagnostic imaging technique that uses high-frequency sound waves to create an image of the internal organs.
Magnetic resonance imaging (MRI). A noninvasive procedure that produces 2-dimensional view of an internal organ or structure, especially the brain and spinal cord. If additional imaging is needed, your doctor may order a PET scan, which can determine where your cancer started.
Barium swallow. Because cancer of the esophagus may occur with oral cancer, your doctor may order this test, often called an upper GI series, to look for cancer of the esophagus. You will drink a chalky solution while X-rays are taken.
Endoscopy. A small fiberoptic scope can be used to to examine the oropharynx and oral cavity. The scope can also be used to obtain biopsies.
Once a diagnosis is made, the cancer will be staged (to determine the extent of the disease) before a treatment plan is established.
What is the treatment for oral and oropharyngeal cancers?
Specific treatment for cancers of the oral cavity and oropharynx will be determined by your health care provider based on:
Your age, overall health, and medical history
Extent of the disease
Your tolerance for specific medications, procedures, or therapies
Expectations for the course of the disease
Your opinion or preference
Treatment may include:
Surgery. Different surgery techniques are used to remove specific types of tumors, including:
Primary tumor resection. Removal of the entire tumor and surrounding area of tissue
Maxillectomy. Removal of the tumor, including part or all of the hard palate (roof of the mouth), if bone is involved
Glossectomy. Removal of the tongue
Mohs' micrographic surgery. Removal of the tumor in "slices" to minimize amount of normal tissue removed (may be considered when the cancer involves the lip)
Laryngectomy. Removal of a large tumor of the tongue or oropharynx, which may involve removing the larynx (voice box).
Neck dissection. If cancer has spread to the lymph nodes in the neck, these lymph nodes may need to be removed as well.
Radiation therapy. Treatment that uses high-energy rays that damage cancer cells and halts the spread of cancer. Radiation therapy is very localized, aimed at only the area where the cancer is present. Radiation therapy may be administered externally with a machine, or internally with radioactive materials.
Chemotherapy. Medications that go throughout the entire body to kill cancer cells. Chemotherapy has the ability to interfere with the cancer cell's replication. Chemotherapy may be used in combination with surgery and radiation therapy.
Targeted therapy. Drugs that target specific cancer cells are also an option and often cause less side effects than chemotherapy that kills both cancerous and noncancerous cells. One such example is cetuximab (Erbitux) that targets epidermal growth factor receptors.
How do people prepare for oral and oropharyngeal cancer surgery?
If surgery is needed to treat the oral and oropharyngeal cancers, the NCI recommends asking the following questions:
What type of operation will I undergo?
What can I expect after surgery?
How will any pain be treated?
Will I have trouble eating? Talking?
Will I have any scarring?
Will there be any long-term effects or permanent physical changes from surgery?
If I need plastic surgery, how soon can that be done following the initial surgery?
Will I need speech therapy?
When can I resume my normal activities?
What are the chances that the cancer will come back?
What are the side effects of treatment for oral and oropharyngeal cancers?
Side effects of treatment vary, depending on the type of treatment and the area being treated. Side effects can be temporary or permanent. The following are some of the more common side effects of treatment for cancers of the oral cavity and oropharynx:
Swelling from surgery
Sore mouth
Difficulty chewing, swallowing, or talking
Changes to appearance, temporarily or permanently
Weight loss due to a sore mouth, which may make eating difficult
Inability to wear dentures for a period of time
Depending on the type of treatment, other side effects may include:
Fatigue
Dental problems
lowered immune system
Nausea
Vomiting
Mouth sores
Lack of appetite
What type of rehabilitation is needed after treatment for oral and oropharyngeal cancers?
Rehabilitation may vary from person to person depending on the type of treatment, and the location and extent of the cancer. Rehabilitation may include:
Dietary counseling. Many patients recovering from surgery have difficulty eating, so it is often recommended that they eat small meals consisting of soft, moist foods.
Surgery. Some patients may benefit from reconstructive or plastic surgery to restore the bones or tissues of the mouth, returning a more normal appearance.
Prosthesis. If reconstructive or plastic surgery is not an option, patients may benefit from dental or facial-part prosthesis to restore a more normal appearance. Special training may be needed to learn to use a prosthetic device.
Speech therapy. If a patient experiences difficulty in speaking following treatment, speech therapy may help the patient relearn the process.
Connect with us:
Download our App: