Choosing a Bariatric Surgery Procedure
What is bariatric surgery?
Bariatric surgery is a type of surgery to help you lose weight. It's a choice for some people who are obese and have not been able to lose weight with other methods. Your healthcare provider might discuss bariatric surgery with you if you are morbidly obese, or if you are obese and have an obesity-related health problem. These include diabetes, sleep apnea, asthma, high blood pressure, and arthritis. Diabetes and certain other health problems may get better with weight loss.
There are several different bariatric surgery procedures. The type of bariatric surgery that works best for you will depend on several factors. These include your general health, your health needs, and your own preference.
What types of bariatric surgeries are available?
The most common types of bariatric surgery are sleeve gastrectomy, gastric bypass, and adjustable gastric banding.
Lap banding is also known as laparoscopic adjustable gastric banding. During lap banding your surgeon places an adjustable band around the top of your stomach. Your surgeon also places a small device called a port under the skin of your stomach. A thin tube leads from the band to the port. Fluid is injected into the port and flows to the band to make it squeeze tighter around the top of the stomach. Fluid can also be removed through the port to loosen the band if it's too tight. The band around your stomach reduces the amount of food that you can eat at one time.
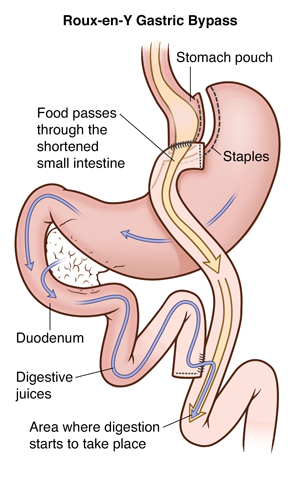
Gastric bypass is another common type of bariatric surgery. It's also called a Roux-en-Y gastric bypass. This surgery also reduces the amount of food you can eat at one time. And it reduces the number of calories and nutrients you can absorb from the foods you eat. During gastric bypass, your surgeon separates part of the stomach to create a small pouch. The pouch is then attached to a part of your small intestine. This small pouch holds less food, making you feel full faster. As food bypasses the rest of the stomach and upper part of your small intestine, you absorb fewer calories and nutrients.
Sleeve gastrectomy is a type of surgery that removes up to 85% of the stomach. It's also known as a gastric sleeve or vertical sleeve gastrectomy. The surgery turns the stomach into a narrow tube that looks like a sleeve. The sleeve holds much less food, and you feel full faster. Your stomach also makes less of one of the hormones that causes hunger.
A less common type of weight-loss surgery is called biliopancreatic diversion with duodenal switch (BPD-DS). In this procedure, your surgeon removes part of the stomach to create a gastric sleeve, as with the sleeve gastrectomy. The sleeve is then attached to a part of the lower small intestine. The sleeve holds much less food, and your body absorbs far fewer calories and nutrients from food.
Surgeons can do most of these types of surgeries as minimally invasive procedures, known as laparoscopic surgery. This type of surgery is done with small incisions, a small camera, and small tools. It's most likely that your surgeon will use a laparoscopic approach for your bariatric surgery.
Surgeons may also do other uncommon types of weight-loss surgery. Your healthcare provider can tell you more if one of these procedures might be better for you.
What are the advantages and disadvantages of each type of bariatric surgery?
Lap banding is a more simple surgery. After lap band surgery, it's fairly easy to loosen or tighten the band, but you may need more visits to your healthcare provider for band adjustments. A tighter band might help you feel fuller sooner. This might help you lose weight more quickly. If you have lap banding, your risk of serious complications right after your surgery is low. This surgery can lead to loss of 40% to 50% of your weight. But results vary a lot between different people. You might not lose as much weight as you would like.
Lap banding might not be right for you if you think you'll have a hard time following a nutritional program. For example, if you drink a lot of high-calorie liquids, the lap band may not help you lose weight. You might develop heartburn or reflux if the band is tight. The band sometimes slips out of position and can cause an obstruction of the stomach. Some bands have to be removed because of this.
Sleeve gastrectomy is more complex than the band, because much of the stomach is removed. Food still travels the same way it did before surgery, and some vitamins like iron and calcium are absorbed almost the same way as before surgery. If you need an upper endoscopy later, the endoscopist can see the same structures. This is different from a gastric bypass, where it's much harder to see other parts of the stomach and the duodenum. You most likely can still take nonsteroidal anti-inflammatory medicines after surgery, although they increase the risk for an ulcer. You may lose from 50 to 100 pounds with a sleeve gastrectomy, if you eat and exercise as you should do.
As time goes by, the sleeve can dilate, or get larger. This means that you could eat more food and gain weight back. Another risk is heartburn or reflux, which can happen after surgery. You might need to take medicines for this. If you already have heartburn or reflux before surgery, doing a sleeve gastrectomy could make it much worse.
Gastric bypass is more complex surgery than sleeve gastrectomy. It works very well for weight loss, and you can lose 100 pounds or more. It's one of the best operations to improve or resolve diabetes, and also is a very good operation to resolve heartburn or reflux. The weight loss goes on for about a year, and then it's usual to see some weight regain. It's very important to keep up with eating the right foods, and to keep physically active. You are also more likely to have problems with nutritional deficiency, and do need to take multivitamins, calcium, and vitamin B-12 regularly. You can get ulcers at the bottom of the stomach pouch if you smoke, or if you take nonsteroidal anti-inflammatory medicines on a regular basis. Because the operation is on the small bowel as well, you might get a small bowel obstruction later in life, and need surgery for that. If you eat the wrong things like sugars, you might have the dumping syndrome (abdominal cramping and diarrhea), but this can usually be avoided by eating the right foods.
A BPD-DS procedure (the duodenal switch) may be most helpful for a person who is extremely obese. You can lose over 150 or 200 pounds with it. It's likely the best operation for diabetes. It also can keep the weight off for many years. It has a higher risk of some complications than other weight-loss surgery. Because fats are not absorbed very well, if you do eat fatty foods, you may have loose bowel movements or diarrhea. You also need to take more vitamins than with a gastric bypass. The duodenal switch has a higher risk of nutritional and vitamin deficiencies. You will need to see your healthcare provider periodically to have check-ups.
What are the risks of bariatric surgery?
All surgery has risks. Your risks may vary according to your general health, your age, the type of surgery you choose, and the amount of weight you need to lose. Talk with your healthcare provider about the risks that most apply to you. Risks of bariatric surgery include:
Bleeding
Infection, including a leak from the staple lines from the stomach or small bowel
Blockage of your bowels (intestinal blockage)
Blood clots in your legs that can travel to your lungs and heart
Heart attack
Need for follow-up surgery
Gallstones (a later complication). This requires surgery to remove the gallbladder.
Nutritional deficiencies from poor absorption (a later complication)
Mental health problems after the procedure
Poor wound healing, including scarring of the incisions, and a hernia at the incisions
Problems with the band or the port that often need more surgery
Gastric reflux
There is also a risk that you might regain weight after you have lost it.
How does surgery compare with medical treatment?
People who get surgery tend to lose much more weight than people who get medical therapy for their weight loss, as long as they follow the recommendations for change in their diet and physical activity. This also means that surgery is more likely to help improve their health conditions linked to obesity, such as diabetes or sleep apnea. Some people can have large weight loss with medical therapy alone, but most morbidly obese people won't be able to keep the weight off. Some people don't lose as much weight as they want after surgery, and some people can regain weight after they have lost it after surgery.
What should I look for in a bariatric surgery program?
Look for an accredited surgery center with a support staff. Support staff should include a dietitian, counselor, and nurses or physician assistants who have had experience in weight loss surgery. Your healthcare provider should be board certified. The center should also provide you with an education program. The program is to help prepare you for before, during, and life after surgery. This is very important to help ensure good results after surgery. The program will likely take several months to prepare you for surgery. And it should provide long-term follow-up after surgery.
How will I need to manage my condition after surgery?
For the rest of your life, you need to work with your healthcare providers to stay healthy. Your medical team will keep track of your health, especially as you lose weight quickly in the first 6 months or so after your surgery. Weight loss tends to be at its peak around a year after surgery.
You will get instructions about how to adapt to your new diet after your surgery. You will likely be on liquid nutrition for a few weeks after surgery. Over time, you'll start to eat soft foods and then solid foods. If you eat too much or too quickly, you may have abdominal pain or vomiting. You'll learn how to know when your new stomach is full.
Your healthcare provider will give you more instructions about your diet. These may vary depending on the type of surgery you had. You'll need to learn good habits like choosing healthy foods and not skipping meals. Your healthcare provider or nutritionist may also need to screen you for low levels of certain nutrients. This is more of a problem with gastric bypass, sleeve gastrectomy, and with BPD-DS surgery.
It's important to have sensible goals about what bariatric surgery might achieve for you. Some people having bariatric surgery have weight loss that does not meet their goals. Even if you don't lose all of your excess weight, medical issues, such as diabetes, sleep apnea, and high blood pressure should get better. You may be able to reduce the amount of medicines that you need to take.
Connect with us:
Download our App: