Nephrostomy Tube
Urine is produced in the kidney and flows down a small tube called the ureter into the bladder. Sometimes the flow of urine is blocked due to stones, infection, congenital abnormalities or trauma. To restore the flow, a nephrostomy tube (small catheter) can be placed through the skin of the lower back into the kidney. As a result, urine will then drain into a small bag connected to the tube. A nephrostomy tube may be in place for days, weeks or months.
Procedure
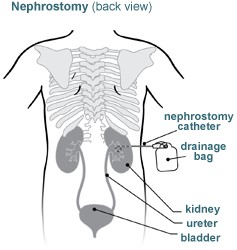
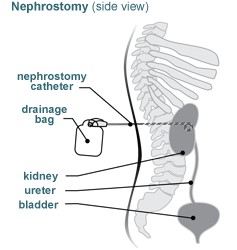
Using ultrasound, the interventional radiologist will locate the kidney and insert a special hollow needle through the skin into the kidney. Using live X-ray (fluoroscopy) for guidance, the doctor will guide a small catheter into the kidney. The portion of the catheter on the outside of the skin will be connected to a drainage bag. A small stitch and/or an adhesive clip will hold the catheter in place on the surface of the skin. The procedure should take approximately an hour to complete.
Your child will be protected by an X-ray shield.
We will place gauze and a clear bandage over the catheter site. Be sure to keep the bandage dry.
Anesthesia
Patients receive either IV sedation or general anesthesia and are asleep for this procedure.
Risks
The procedure is considered low-risk. However, potential complications include:
- bleeding
- infection
- injury to the kidney, ureter or bladder
- allergic reaction to the X-ray dye (contrast reaction)
Pain
The catheter site may be tender for several days.
Bathing
In addition to the gauze and a clear bandage over the catheter site, the catheter will be secured with a StatLock® locking device which must not be removed. The bandage must remain dry and in place at all times. You may sponge-bathe your child, but must keep the site dry.
Activity Restrictions
Your child must avoid activities such as contact sports or rough playing which may result in a pull to the catheter and damage to or loss of the catheter.
Connect with us:
Download our App: