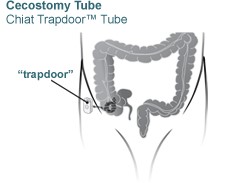
Cecostomy Tube
Patients with fecal incontinence can use a cecostomy tube to administer an enema to quickly and completely evacuate the large intestines through the anus. The tube is a catheter (a small tube) placed into the cecum, the first part of the large bowel in the lower right abdomen.
Procedure
Before the procedure, the patient must follow a “bowel prep” to cleanse the colon. Proper bowel preparation is important for successful placement of a cecostomy tube. (Details are on this page.)
The doctor begins the procedure by inflating the colon with air until the cecum is distended. The doctor inserts a small needle through the skin into the cecum, and then attaches the bowel to the abdominal wall with two stitches. A catheter is then threaded through a special hollow needle into the cecum. To confirm proper placement of the catheter, we will inject contrast dye through the catheter, using live X-ray (fluoroscopy) to make sure the dye travels into the cecum. Your child will be protected by an X-ray shield during the procedure.
Anesthesia
Patients receive either IV sedation or general anesthesia and are asleep for this procedure.
Risks
The procedure is considered low-risk. However, potential complications include:
- peritonitis (infection in the abdomen)
- abscess (infected fluid collection)
- bleeding
- injury to the colon and/or surrounding structures
Preparation before Procedure
Your child must follow a clear-fluid diet for two days before the procedure. (We will provide you with detailed instructions.) The night before, your child will drink sodium phosphate oral solution, a laxative to help clean out the bowel. On the day of the procedure, your child will have an abdominal X-ray to determine whether the bowel is clean of stool. A repeat dose of sodium phosphate may be required.
After the Procedure
Most children are hospitalized for two to three days to minimize the risk of complications. Your child will receive IV antibiotics while in the hospital, and we will give you a prescription for oral antibiotics at discharge. Your child will be allowed to move around as tolerated. The catheter insertion site may be tender for several days.
A clear-liquid diet must be continued until normal bowel function returns. This may take several days. We will provide detailed instructions in person.
Your child’s doctor will talk about the proper bowel-cleansing regimen with you based on your child’s unique needs. Usually you can start administering enemas through the tube after approximately one week.
The tube will be removed two months after it is placed. It will be replaced with a low-profile tube, called a Chait Trapdoor, which sits on the surface of the skin. Routine changes of this tube will be performed once or twice a year.
Connect with us:
Download our App: