The Stanford Medicine Children’s Health Fetal and Pregnancy Health Program’s team of specialists in maternal-fetal medicine, pediatric radiology, neonatology, pediatric neurosurgery, and pediatric surgery provide multidisciplinary evaluation, consultation, and therapy for fetal spina bifida.
What is fetal spina bifida?
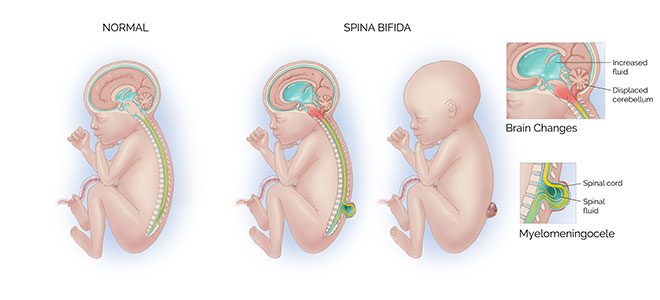
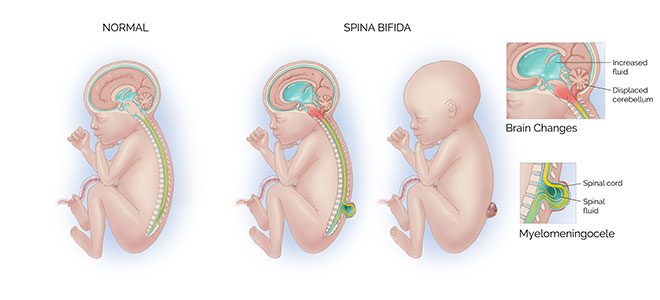
Spina bifida is a condition that happens when the fetus’s bony spine, which protects the spinal cord and nerves, doesn’t develop normally. The spinal cord and nerves are then exposed to the amniotic cavity, which leads to their ongoing damage during pregnancy. Due to this nerve damage, children with severe forms of spina bifida have difficulty with walking, and with bowel and bladder function.
Spina bifida also can cause the developing brain to herniate into the base of the skull, creating fluid buildup within the brain.
- This herniation is known as a Chiari II malformation, and increased fluid buildup in the brain is called hydrocephalus.
- Children with spina bifida often require a ventriculoperitoneal shunt or endoscopic third ventriculostomy after delivery in order to reduce the fluid in the brain and relieve the pressure that can build up in the skull.
How common is fetal spina bifida?
Fetal spina bifida affects 3 to 4 out of 10,000 live births in the United States.
How is spina bifida diagnosed?
Spina bifida can be tested with maternal blood tests, but the diagnosis is usually made with an ultrasound.
What are the most common types of spina bifida?
- Spina bifida occulta. A mild form of spina bifida in which the skin covers the spinal defect, and the spinal cord and the nerves do not herniate into the amniotic cavity. This form of spina bifida may be characterized only by a hairy patch, dimple, or birthmark over the area of the defect after delivery. Some babies with this condition require surgery at 3 to 6 months of age to de-tether the spinal cord.
- Lipomyelomeningocele. A moderate form of spina bifida in which the skin covers the spinal defect, but there is a fatty lump under the skin that is tethered to the spinal cord. Infants with this condition require surgery at 3 to 6 months of age to repair the defect.
- Meningocele. A moderate form of spina bifida in which only a fluid-filled sac herniates outside the spine, and the spinal nerves do not. This condition may require early repair after birth or in the first six months of the patient’s life, depending on the skin overlying the meningocele.
- Myelomeningocele. A severe form of spina bifida in which the nerves herniate through the bony defect outside of the body and are covered by a thin fluid-filled sac. The nerves that are exposed to the amniotic cavity are damaged over time, leading to difficulty walking and problems with bladder and bowel function.
How does the Packard Children’s Hospital team typically provide care for fetal spina bifida?
We offer patients in utero spina bifida repair either through open fetal surgery or a minimally invasive fetoscopic approach under a Stanford Institutional Review Board–approved study.
The traditional approach of in utero repair is done through open fetal surgery.
- This approach has been validated using a large prospective clinical trial that highlighted significant neonatal benefits.
- Unfortunately, because of the uterine incision, open fetal surgery carries risks to the mother, including bleeding, pulmonary edema, a thinning of the uterine incision during the pregnancy, a need for cesarean delivery in the current and all future pregnancies, preterm rupture of the membranes, preterm delivery, and traumatic uterine rupture during future pregnancies.
While still in the investigational stages, fetoscopic fetal spina bifida repair may lower the risks of the traditional form of repair by reducing the need for a uterine incision. Other benefits include faster maternal recovery, potential for vaginal trial of labor, and potential for delivery at later gestational ages, as compared with open fetal surgery.
When is an in utero repair performed?
- Isolated spinal lesion starting at or above S1.
- Chiari II malformation (herniation of the posterior fossa [cerebellum] into the base of the skull).
- Surgery must be performed before 25 6/7 weeks.
- Normal karyotype or microarray testing via amniocentesis.
- No contraindications to in utero surgery—no prior myomectomy or any surgery on the uterus (other than cesarean).
- Low risk for preterm birth—no history of preterm birth, normal cervical length.
- Evaluation includes ultrasound, MRI, fetal echocardiogram, amniocentesis, and multidisciplinary consultation.
What problems can fetal spina bifida cause after birth?
Spina bifida could be associated with long-term complications, including paralysis, the inability to walk, excess fluid on the brain (hydrocephalus), neurocognitive delays, deformities, and neurocognitive disability. However, prenatal surgery can improve overall outcomes, such as an improved ability to walk independently and better neuromotor development.
About fetal spina bifida (PDF) >
Connect with us:
Download our App: