Chronic Inflammatory Demyelinating Polyradiculoneuropathy
What is chronic inflammatory demyelinating polyradiculoneuropathy?
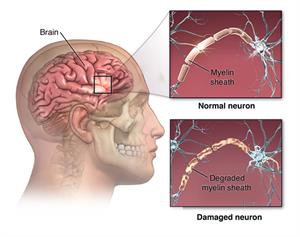
Chronic inflammatory demyelinating polyradiculoneuropathy (CIDP) is a rare type of autoimmune disorder. In an autoimmune disease, the body attacks its own tissues. In CIDP, the body attacks the myelin sheaths. These are the fatty coverings on the fibers that insulate and protect the nerves.
Experts think that CIDP is related to the more commonly known disease Guillain-Barré syndrome (GBS). GBS is generally considered more of an acute, or short-term, disease. CIDP is considered a chronic, or long-term, disease. CIDP is less common than GBS.
CIDP is usually classified as follows:
Progressive. The disease continues to worsen over time.
Recurrent. Episodes of symptoms stop and start.
Monophasic. This means one bout of the disease lasts 1 to 3 years and doesn’t recur.
What causes CIDP?
CIDP occurs when the body's immune system attacks the myelin sheaths around nerve cells. But exactly what triggers this is not clear. Unlike GBS, there is usually no infection preceding CIDP. There does not seem to be a genetic link to CIDP.
Who is at risk for CIDP?
CIDP can occur in anyone. But people in their 50s and 60s seem more likely to develop it than other age groups. Men are twice as likely as women to get the disease.
What are the symptoms of CIDP?
Regardless of the type of CIDP you may have, symptoms are usually the same. They can include:
Tingling in your arms and legs
Gradual weakening of your arms and legs
Loss of reflexes
Loss of balance and your ability to walk
Loss of feeling in your arms and legs, which often starts with your inability to feel a pin prick
How is CIDP diagnosed?
Because CIDP is rare, it’s often hard to correctly diagnose the disease, at least at first. Healthcare providers can confuse its symptoms with those of GBS, because of the similarity between the diseases. If symptoms last longer than 8 weeks, your healthcare provider may suspect CIDP.
After taking your medical history and doing a physical exam, your healthcare provider may do other tests to confirm a diagnosis including:
Blood and urine tests
A nerve conduction study to look for myelin damage in peripheral nerves. This test is sometimes called an electromyogram. It involves using low electrical currents to test nerve function and response.
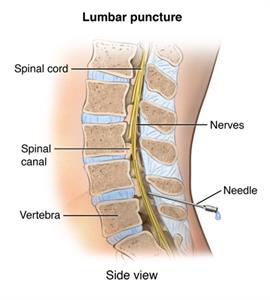
A lumbar puncture. In this procedure, a small needle is inserted into your back and a sample of your cerebrospinal fluid (CSF) is withdrawn. CSF is the fluid that surrounds your spinal cord. The procedure helps healthcare providers detect elevated levels of certain proteins related to the disease.
How is CIDP treated?
Treatment for CIDP is often effective. Some studies show that up to 80% of people respond well to therapy. Because it is an autoimmune disorder, healthcare providers use medicines that suppress your immune response to treat CIDP. Your medical team tailors your treatment to you and closely monitors your progress. Treatments for CIDP include:
Immunosuppresive medicines
Steroids
Intravenous immunoglobulin
Plasma exchange (plasmapheresis) to remove immune system proteins from the blood
Living with CIDP
The course of CIDP can vary greatly between different people, as can the response to treatment.
Getting treatment as early as possible is very important because it gives you the best chance of limiting symptoms and keeping this condition under control. If you do not seek treatment for CIDP, your symptoms will likely get worse over the course of several years. These can range from sensory symptoms, such as tingling and numbness, to weakness and loss of balance. Without treatment, 1 in 3 people with CIDP will need a wheelchair.
In people with permanent physical impairments, physical therapy can be very important. In this treatment, specialists will work with you to maintain or increase your strength and improve your coordination. Another type of therapy is occupational therapy. It helps you learn new ways of doing everyday tasks in spite of your new physical limitations.
Some people with physical disabilities often feel sad or depressed. If this happens to you, your healthcare provider may recommend that you see a mental health provider. Antidepressants and psychotherapy can help treat depression. So can support groups for people managing chronic health conditions.
When should I call my healthcare provider?
If you have been diagnosed with CIDP, talk with your healthcare provider about when you might need to call them. They will likely advise you to call if you notice worsening of any symptoms or if you develop any new symptoms.
Key points about chronic inflammatory demyelinating polyradiculoneuropathy
Chronic inflammatory demyelinating polyradiculoneuropathy (CIDP) is a slowly developing autoimmune disorder in which the body's immune system attacks the myelin that insulates and protects your body’s nerves. The exact cause is not known.
Common symptoms are gradual weakness or sensation changes in the arms or legs. This might get worse over time, or it might come and go.
Early treatment is important to limit disease progression. It includes medicines or other treatments to suppress the immune system.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
Know the reason for your visit and what you want to happen.
Before your visit, write down questions you want answered.
Bring someone with you to help you ask questions and remember what your provider tells you.
At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
Ask if your condition can be treated in other ways.
Know why a test or procedure is recommended and what the results could mean.
Know what to expect if you do not take the medicine or have the test or procedure.
If you have a follow-up appointment, write down the date, time, and purpose for that visit.
Know how you can contact your provider if you have questions.
Connect with us:
Download our App: